Overview:
A stroke is a medical emergency that occurs when the blood supply to a part of the brain is interrupted or reduced, preventing brain tissue from receiving the oxygen and nutrients it needs.
This interruption can lead to brain cells dying within minutes, causing significant damage to brain function and potentially leading to disability or death.
Often referred to as a “brain attack,” a stroke is one of the leading causes of mortality and long-term disability worldwide.
However, with prompt treatment and lifestyle modifications, the risk of stroke can be minimized.
This blog will provide an in-depth look at stroke, including its symptoms, causes, risk factors, treatment options, and preventive measures.
Table of Contents
What is a Stroke?
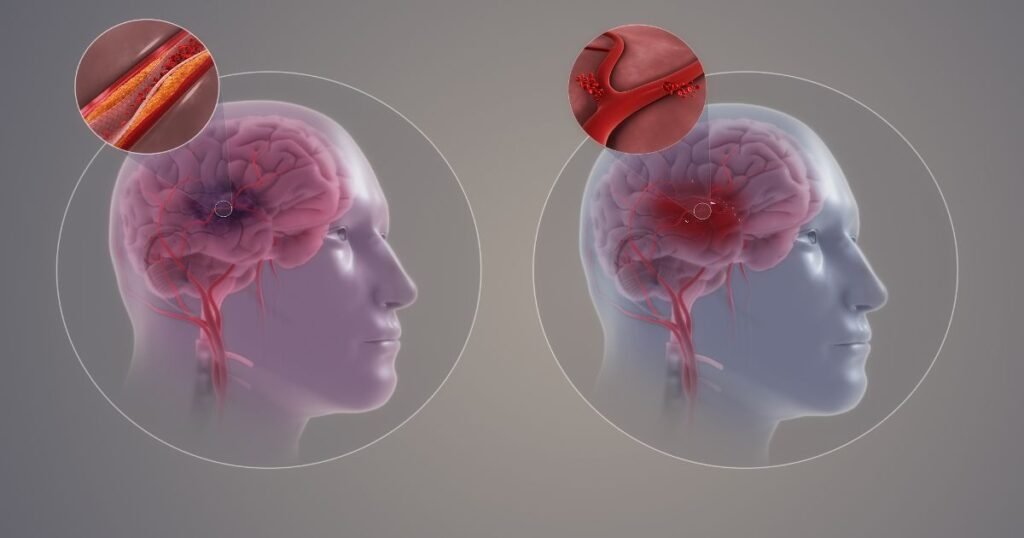
A stroke happens when the blood supply to part of the brain is interrupted or reduced, depriving brain tissue of essential oxygen and nutrients. There are two main types of stroke:
There are two main types of stroke:
1. Ischemic Stroke: This is the most common type, accounting for about 87% of all strokes. It occurs when a blood clot blocks or narrows a blood vessel in the brain. This blockage can be caused by a blood clot that forms in the brain’s blood vessels (thrombotic stroke) or a clot that forms elsewhere in the body and travels to the brain (embolic stroke).
2. Hemorrhagic Stroke: This type occurs when a blood vessel in the brain ruptures, leading to bleeding in or around the brain. Hemorrhagic strokes can result from high blood pressure, aneurysms, or trauma.
In addition to these, there is a condition known as a Transient Ischemic Attack (TIA) or “mini-stroke.” A TIA occurs when blood flow to the brain is temporarily blocked.
Although the symptoms last only a few minutes to hours and cause no permanent damage, it is a warning sign of a potential future stroke and should not be ignored.
Symptoms of Stroke
Recognizing the signs and symptoms of a stroke is crucial for receiving timely treatment and preventing severe brain damage. The symptoms usually appear suddenly and can include:
- Sudden Numbness or Weakness: This typically affects one side of the body, especially in the face, arm, or leg.
- Confusion or Trouble Speaking: Difficulty understanding speech, slurred speech, or trouble finding words are common symptoms.
- Vision Problems: Blurred, double vision, or complete loss of vision in one or both eyes can occur.
- Severe Headache: A sudden and intense headache, especially if accompanied by vomiting or altered consciousness, may indicate a hemorrhagic stroke.
- Dizziness or Loss of Balance: Difficulty walking, lack of coordination, or unexplained falls may be signs of a stroke.
- Difficulty Swallowing: In some cases, individuals may have trouble swallowing or experience drooling.
Remember FAST: An easy way to recognize the most common symptoms of stroke is by using the acronym FAST:
- Face drooping: Is one side of the face drooping or numb?
- Arm weakness: Is one arm weak or numb?
- Speech difficulty: Is speech slurred, or is the person unable to speak or hard to understand?
- Time to call emergency services: If you observe any of these symptoms, seek immediate medical attention and call your local emergency number(of your country or region).

Causes of Stroke
The underlying cause of a stroke depends on its type:
Ischemic Stroke: This occurs due to a blood clot or buildup of fatty deposits (plaque) in the arteries. Common causes include:
- Atherosclerosis: The buildup of plaque in the arteries that narrows blood vessels, reducing blood flow.
- Blood Clots: Blood clots can form due to irregular heart rhythms like atrial fibrillation, increasing the risk of an ischemic stroke.
Hemorrhagic Stroke: This type results from bleeding in the brain caused by:
- High Blood Pressure (Hypertension): Chronic high blood pressure can weaken blood vessels in the brain.
- Aneurysms: Aneurysms, which are bulging blood vessels, can burst and cause bleeding.
- Arteriovenous Malformations (AVMs): These are abnormal tangles of blood vessels that can rupture.
Transient Ischemic Attack (TIA): TIAs are caused by temporary blockages that reduce blood flow to the brain. They often serve as warning signs for a more severe stroke.
Risk Factors of Stroke
Several risk factors can increase the likelihood of having a stroke. These risk factors can be categorized into controllable and uncontrollable factors:
Controllable Risk Factors:
- High Blood Pressure: Hypertension is the leading cause of stroke. Managing blood pressure through lifestyle changes or medication can reduce the risk.
- Diabetes: People with diabetes are more likely to develop blood clots, increasing their risk of stroke.
- High Cholesterol: Elevated cholesterol levels can lead to plaque buildup in the arteries, narrowing blood vessels.
- Heart Disease: Conditions like atrial fibrillation or congestive heart failure increase the risk of blood clots.
- Obesity: Excess weight contributes to conditions like hypertension, diabetes, and high cholesterol.
- Smoking: Smoking damages blood vessels and thickens blood, increasing the risk of clot formation.
- Excessive Alcohol Consumption: Drinking large amounts of alcohol can raise blood pressure and lead to stroke.
Uncontrollable Risk Factors:
- Age: The risk of stroke increases with age, especially after 55.
- Gender: Men are more likely to have a stroke at a younger age, while women have a higher lifetime risk.
- Family History: A family history of stroke or heart disease increases the risk.
- Previous Stroke or TIA: Individuals who have had a stroke or TIA are at higher risk of another stroke.
Treatment for Stroke
The treatment for stroke depends on the type and severity of the condition. Immediate treatment is essential to minimize brain damage and improve outcomes.
Emergency Treatment for Ischemic Stroke:
- Clot-Busting Medications: Tissue plasminogen activator (tPA) is a medication that can dissolve blood clots if administered within 4.5 hours of symptom onset.
- Mechanical Thrombectomy: This procedure involves using a catheter to remove the blood clot from the blocked artery. It is typically performed within 6 to 24 hours of symptom onset.
Emergency Treatment for Hemorrhagic Stroke:
- Medications: Medications may be given to control blood pressure, prevent seizures, and reduce bleeding.
- Surgery: In some cases, surgery may be required to repair the ruptured blood vessel, remove blood clots, or relieve pressure on the brain.
Post-Stroke Rehabilitation:
Rehabilitation plays a crucial role in helping individuals recover and regain as much function as possible. Rehabilitation may include:
- Physical Therapy: Helps improve muscle strength, coordination, and mobility.
- Speech Therapy: Assists with speech, language, and swallowing difficulties.
- Occupational Therapy: Focuses on regaining the ability to perform daily activities.
- Psychological Support: Counseling or therapy can help individuals cope with emotional changes following a stroke.
Prevention of Stroke
Preventing a stroke involves managing risk factors and making lifestyle changes to promote overall health:
- Maintain a Healthy Diet: A diet rich in fruits, vegetables, whole grains, proteins, and low-fat dairy can help maintain a healthy weight and reduce blood pressure and cholesterol levels.
- Exercise Regularly: Regular physical activity, such as brisk walking, swimming, or cycling, can help lower blood pressure, control weight, and reduce stress.
- Manage Blood Pressure and Cholesterol Levels: Monitoring and controlling blood pressure and cholesterol can reduce the risk of stroke.
- Quit Smoking: Stopping smoking improves heart and vascular health and decreases the risk of stroke.
- Avoid Alcohol Intake: Avoiding alcohol can help prevent high blood pressure and reduce the risk of stroke.
- Control Blood Sugar Levels: For those with diabetes, keeping blood sugar levels in check is essential to reduce stroke risk.
- Take Medications as Prescribed: If you have been prescribed medication for high blood pressure, high cholesterol, or diabetes, it is crucial to take them as directed by your healthcare provider.

Key Takeaways
A stroke is a devastating medical emergency that can have lifelong consequences.
However, by understanding the causes, symptoms, and risk factors, individuals can take proactive steps to reduce their risk.
Recognizing the signs and seeking immediate medical attention can significantly improve outcomes and save lives.
Prevention is key, and adopting a healthy lifestyle, managing chronic conditions, and undergoing regular health checkups are vital in reducing the risk of stroke.
With the right knowledge and preparation, the impact of stroke can be minimized, and individuals can lead healthier lives.
FAQs
1. What is the difference between a stroke and a heart attack?
A stroke occurs when the blood supply to a part of the brain is interrupted, whereas a heart attack is caused by a blockage in the coronary arteries, which supply blood to the heart muscle.
2. Can a stroke be completely prevented?
While not all strokes can be prevented, maintaining a healthy lifestyle and managing risk factors like high blood pressure, diabetes, and high cholesterol can significantly reduce the risk.
3. What should I do if I suspect someone is having a stroke?
If you suspect someone is having a stroke, act FAST. Check for symptoms like face drooping, arm weakness, and speech difficulties, then call emergency services immediately. The quicker they receive medical attention, the better the chances of minimizing brain damage.
4. Can younger people have strokes?
Yes, although the risk of stroke increases with age, younger people can also have strokes. Certain conditions like high blood pressure, diabetes, smoking, and heart disorders can increase the risk of stroke in younger individuals.
5. What is a Transient Ischemic Attack (TIA)?
A Transient Ischemic Attack (TIA), often called a “mini-stroke,” occurs when the blood flow to the brain is temporarily blocked. The symptoms are similar to those of a stroke but typically last for only a few minutes to hours and do not cause permanent damage. However, a TIA is a warning sign of a potential future stroke and should be taken seriously.
6. How long does it take to recover from a stroke?
Stroke recovery varies widely depending on the severity of the stroke and the areas of the brain affected. Some people recover within weeks or months, while others may require years of rehabilitation. Early intervention and rehabilitation can improve recovery outcomes.
7. Can stress lead to a stroke?
While stress alone may not directly cause a stroke, it can contribute to risk factors like high blood pressure and unhealthy behaviors (e.g., smoking, and overeating), which increase the likelihood of having a stroke.
8. What lifestyle changes can reduce the risk of a second stroke?
Lifestyle changes that can help reduce the risk of a second stroke include:
- Adopting a heart-healthy diet (low in saturated fats, trans fats, and cholesterol)
- Engaging in regular physical activity
- Managing blood pressure, cholesterol, and diabetes effectively
- Quitting smoking and limiting alcohol consumption
- Taking prescribed medications as directed by your healthcare provider
9. Can a person live a normal life after a stroke?
Yes, with the right medical care, rehabilitation, and support, many stroke survivors can lead fulfilling and active lives. The extent of recovery depends on the severity of the stroke and the effectiveness of post-stroke rehabilitation.
10. Are there specific warning signs before a stroke occurs?
Some people may experience warning signs like sudden vision changes, dizziness, or difficulty speaking in the days or weeks leading up to a stroke. Paying attention to these warning signs and seeking medical advice can help prevent a full-blown stroke.

