Overview:
Type 1 diabetes, previously known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
This results in little or no insulin production, a hormone that is essential for regulating blood sugar levels. Without insulin, glucose cannot enter the cells to provide energy, leading to high blood sugar levels, which can cause various complications if left untreated.
Although Type 1 diabetes can develop at any age, it often appears during childhood or adolescence, hence the earlier term “juvenile diabetes.” It requires lifelong management, including daily insulin therapy, careful monitoring of blood sugar levels, and a balanced diet.
Unlike Type 2 diabetes, which is often associated with lifestyle factors such as diet and exercise, Type 1 diabetes is an autoimmune condition with complex genetic and environmental triggers.
This blog will delve into the nature of Type 1 diabetes, its symptoms, causes, risk factors, treatment options, prevention strategies, and common FAQs to help individuals and families better understand and manage this condition.
Table of Contents
What is Type 1 Diabetes?
Type 1 diabetes is an autoimmune disease in which the immune system attacks and destroys the insulin-producing beta cells in the pancreas.
Insulin is crucial for allowing glucose (sugar) from the food we eat to enter cells and provide energy. When insulin production ceases or becomes insufficient, blood sugar levels increase, leading to hyperglycemia (high blood sugar).
If left unmanaged, this condition can lead to severe complications, including heart disease, kidney damage, nerve damage, and vision problems.
The onset of Type 1 diabetes is usually sudden and can occur in both children and adults. Individuals with Type 1 diabetes need to manage their blood sugar levels through regular insulin injections or the use of an insulin pump.
They must also monitor their blood glucose levels, follow a healthy diet, engage in physical activity, and work closely with healthcare professionals to maintain optimal health.
Types of diabetes:
There are three main types of diabetes:
- Type 1 Diabetes: In type 1 diabetes, your immune system mistakenly attacks and destroys the beta cells in your pancreas that produce insulin. This damage is permanent and your body will not produce any insulin. 5 to 10% of people with diabetes have type 1 diabetes.
- Type 2 Diabetes: In type 2 diabetes, your body’s cells become less responsive to insulin. 90 to 95% of people with diabetes have type 2 diabetes.
- Gestational diabetes: This type of diabetes only develops during pregnancy. It usually goes away after giving birth.
Symptoms of Type 1 Diabetes:
The symptoms of Type 1 diabetes can develop rapidly, within a few weeks or months. Recognizing these symptoms early is essential for prompt diagnosis and treatment. Common symptoms include:
- Frequent Urination (Polyuria): Elevated blood sugar levels cause the kidneys to filter out excess glucose, leading to increased urination.
- Excessive Thirst (Polydipsia): Frequent urination can cause dehydration, prompting individuals to feel extremely thirsty.
- Increased Hunger (Polyphagia): Despite eating more than usual, individuals with Type 1 diabetes may feel constantly hungry because their cells are not receiving enough glucose for energy.
- Unexplained Weight Loss: Due to the lack of insulin, the body starts breaking down fat and muscle for energy, resulting in sudden weight loss.
- Fatigue and Weakness: The lack of glucose in cells can cause persistent tiredness and weakness.
- Blurred Vision: High blood sugar can cause the lens of the eye to swell, leading to temporary blurred vision.
- Irritability or Mood Changes: Fluctuations in blood sugar levels can lead to mood swings, irritability, or depression.
- Slow-Healing Wounds: High blood sugar can impair circulation and immune response, causing slow wound healing and increased susceptibility to infections.
- Bed-Wetting in Children: Children who have been toilet-trained may start wetting the bed again due to high blood sugar levels.
If you or your child experience these symptoms, it is crucial to seek medical attention immediately. Early diagnosis and intervention can help manage Type 1 diabetes effectively and prevent complications.
Causes of Type 1 Diabetes:
The exact cause of Type 1 diabetes is not fully understood, but it is believed to be a result of a combination of genetic and environmental factors.
Potential Causes and Contributing Factors:
- Genetic Predisposition: Certain genes are associated with an increased risk of developing Type 1 diabetes. Having a family history of the condition can raise the likelihood, although many people with Type 1 diabetes have no family history.
- Autoimmune Reaction: In Type 1 diabetes, the body’s immune system attacks its own cells. It is unclear what triggers this autoimmune reaction, but it may be influenced by environmental factors such as viral infections or exposure to certain toxins.
- Viral Infections: Some researchers believe that viral infections, such as enteroviruses or the Coxsackievirus, may trigger the onset of Type 1 diabetes in genetically susceptible individuals.
- Environmental Factors: Exposure to certain environmental factors, such as a lack of vitamin D or early introduction of cow’s milk in infancy, has been suggested as potential triggers for the autoimmune reaction.
- Other Factors: Certain medical conditions, such as celiac disease or autoimmune thyroid disease, are more common in individuals with Type 1 diabetes, indicating a possible link between autoimmune disorders.
Risk Factors for Type 1 Diabetes:
Although the exact cause of Type 1 diabetes is unknown, several factors can increase the risk of developing the condition:
- Family History: Having a parent, sibling, or close relative with Type 1 diabetes increases the risk, though the majority of people with Type 1 diabetes have no family history.
- Genetics: Specific genes, such as those in the human leukocyte antigen (HLA) complex, are associated with an increased risk of Type 1 diabetes.
- Age: While Type 1 diabetes can develop at any age, it is more common in children and young adults, with peak incidence occurring between ages 4 and 7 and again between 10 and 14.
- Geography and Ethnicity: Type 1 diabetes is more prevalent in certain geographic regions and ethnic groups. It is more common in people of European descent and less common in individuals of African, Hispanic, or Asian descent.
- Presence of Autoantibodies: Individuals with specific autoantibodies in their blood are at higher risk of developing Type 1 diabetes, even if they do not yet have symptoms.
Treatment for Type 1 Diabetes:
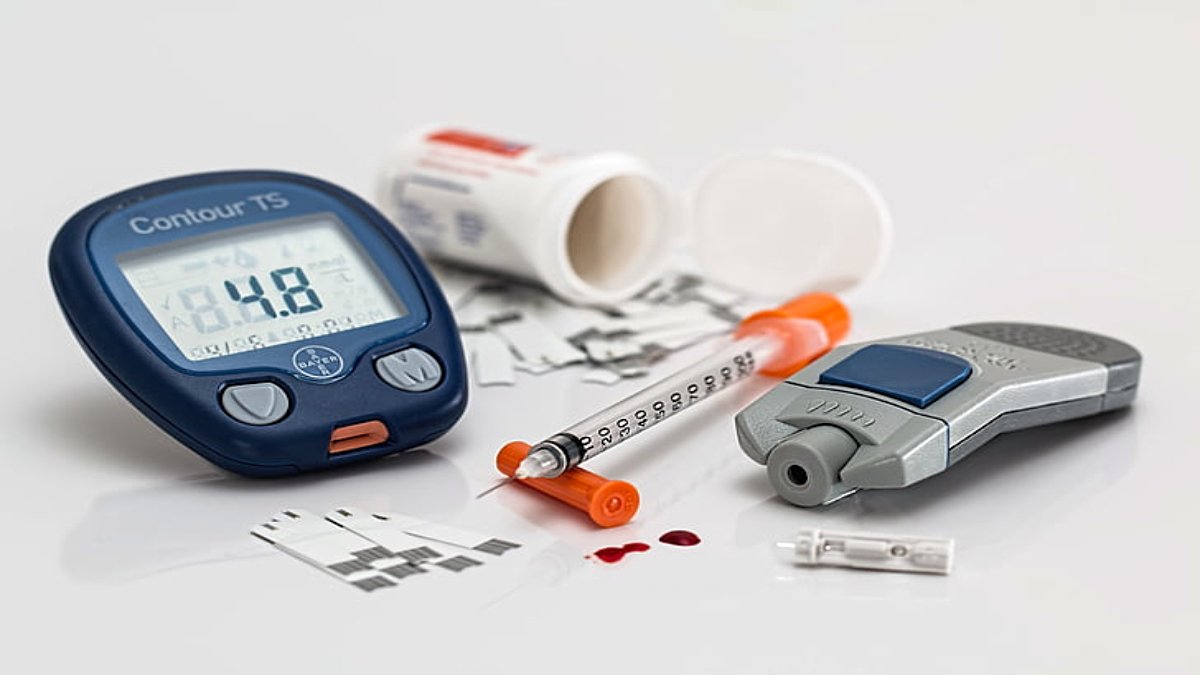
Managing Type 1 diabetes requires a comprehensive approach that includes insulin therapy, blood sugar monitoring, diet, exercise, and education. Since the body is unable to produce insulin, people with Type 1 diabetes must rely on external sources of insulin to regulate their blood sugar levels.
Key Components of Type 1 Diabetes Treatment:
- Insulin Therapy: Individuals with Type 1 diabetes require insulin therapy for life. Insulin can be administered through injections using syringes, insulin pens, or insulin pumps. Different types of insulin are used, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin, depending on individual needs.
- Blood Sugar Monitoring: Regular blood sugar monitoring is essential for managing Type 1 diabetes. Monitoring can be done using a blood glucose meter or a continuous glucose monitor (CGM) that tracks blood sugar levels in real-time.
- Diet and Nutrition: A balanced diet that includes carbohydrates, proteins, and healthy fats is crucial for maintaining stable blood sugar levels. Carbohydrate counting and glycemic index considerations are often used to plan meals.
- Physical Activity: Regular physical activity helps improve insulin sensitivity and overall health. However, exercise can affect blood sugar levels, so individuals with Type 1 diabetes need to monitor their levels before, during, and after exercise.
- Education and Support: Education about diabetes management is vital for individuals and families. Diabetes educators, dietitians, and healthcare providers can offer guidance on insulin management, diet planning, and problem-solving skills.
- Medications for Co-Existing Conditions: Some individuals with Type 1 diabetes may also require medications for other conditions such as high blood pressure or high cholesterol.
- Emergency Treatments: In the event of severe hypoglycemia (low blood sugar) or diabetic ketoacidosis (DKA), immediate treatment is required. Injectable glucagon can be used to treat severe hypoglycemia, while DKA requires hospitalization for intravenous fluids, electrolytes, and insulin therapy.
Prevention of Type 1 Diabetes:
Currently, there is no known way to prevent Type 1 diabetes. However, research is ongoing to better understand the condition and develop preventive strategies. Some approaches being explored include:
- Identifying High-Risk Individuals: Screening for autoantibodies associated with Type 1 diabetes can identify individuals at high risk, allowing for close monitoring and early intervention.
- Immunotherapy: Experimental immunotherapy treatments aim to modify or suppress the autoimmune response that leads to Type 1 diabetes. While promising, these treatments are not yet widely available.
- Environmental Modifications: Some research suggests that modifying environmental factors, such as improving vitamin D levels in early childhood, may reduce the risk of developing Type 1 diabetes.
- Lifestyle Considerations: For those at high risk, maintaining a healthy lifestyle with a balanced diet, regular exercise, and stress management can support overall health and well-being.
Conclusion:
Type 1 diabetes is a complex and lifelong condition that requires continuous management and care.
Early diagnosis and intervention, along with a comprehensive treatment plan that includes insulin therapy, diet, exercise, managing stress, and education, can help individuals with Type 1 diabetes lead healthy and fulfilling lives.
While there is currently no cure or way to prevent Type 1 diabetes, ongoing research offers hope for better understanding, improved treatments, and potential preventive strategies in the future.
Raising awareness about Type 1 diabetes and supporting those affected by the condition can make a significant difference in the quality of life for individuals and their families.
With advances in technology, medical research, and healthcare practices, the outlook for managing Type 1 diabetes continues to improve, providing new opportunities for effective management and long-term health.
FAQs:
1. What is the difference between Type 1 and Type 2 diabetes?
Type 1 diabetes is an autoimmune condition in which the body destroys its insulin-producing cells, leading to a lack of insulin production. Type 2 diabetes, on the other hand, is often related to lifestyle factors such as obesity and physical inactivity and is characterized by insulin resistance and impaired insulin production.
2. Can Type 1 diabetes be cured?
Currently, there is no cure for Type 1 diabetes. However, ongoing research and advancements in treatments aim to improve management and quality of life for individuals with the condition.
3. How is Type 1 diabetes diagnosed?
Type 1 diabetes is diagnosed through blood tests that measure blood glucose levels and the presence of specific autoantibodies.
4. Is Type 1 diabetes hereditary?
While there is a genetic component to Type 1 diabetes, it is not solely hereditary. The presence of certain genes can increase the risk, but environmental factors, such as viral infections, also play a role. Not everyone with a family history of Type 1 diabetes will develop the condition, and many people with the condition do not have a family history.
5. Can Type 1 diabetes be prevented?
As of now, there is no proven way to prevent Type 1 diabetes. Researchers are exploring methods to identify individuals at high risk and develop strategies to prevent or delay the onset of the disease.
6. What are the complications of uncontrolled Type 1 diabetes?
Poorly managed Type 1 diabetes can lead to both short-term and long-term complications. Short-term complications include hypoglycemia (low blood sugar) and diabetic ketoacidosis (DKA), both of which require immediate medical attention. Long-term complications include cardiovascular disease, kidney damage (nephropathy), nerve damage (neuropathy), eye damage (retinopathy), and an increased risk of infections.
7. How often should blood sugar levels be checked?
The frequency of blood sugar monitoring varies depending on individual needs and treatment plans. Typically, individuals with Type 1 diabetes check their blood sugar levels multiple times a day, including before meals, after meals, before and after exercise, and at bedtime. Continuous glucose monitors (CGMs) can provide real-time data and reduce the need for frequent finger pricks.
8. What are the latest advancements in Type 1 diabetes management?
Advancements in technology, such as continuous glucose monitors (CGMs) and insulin pumps, have significantly improved the management of Type 1 diabetes. Researchers are also exploring the potential of artificial pancreas systems, stem cell therapies, and immunotherapy treatments to enhance the quality of life for individuals with Type 1 diabetes.
9. What should people with Type 1 diabetes eat?
A balanced diet that includes carbohydrates, proteins, and healthy fats is recommended for individuals with Type 1 diabetes. Carbohydrate counting and understanding the glycemic index of foods can help manage blood sugar levels. It’s essential to consult a dietitian or diabetes educator to develop a personalized meal plan that meets nutritional needs and aligns with insulin therapy.
10. Can people with Type 1 diabetes lead a normal life?
Yes, with proper management, people with Type 1 diabetes can lead healthy and active lives. Regular monitoring of blood sugar levels, adherence to insulin therapy, a balanced diet, and an active lifestyle are essential components of effective management. Support from healthcare professionals, family, and the community also plays a significant role in improving quality of life.
11. What is diabetic ketoacidosis (DKA)?
Diabetic ketoacidosis (DKA) is a serious complication of Type 1 diabetes that occurs when the body lacks enough insulin to use glucose for energy and begins breaking down fat instead. This process produces ketones, which can build up to dangerous levels in the blood, leading to symptoms such as excessive thirst, frequent urination, nausea, vomiting, abdominal pain, confusion, and fruity-smelling breath. DKA requires immediate medical attention and hospitalization.
12. How does exercise impact Type 1 diabetes management?
Exercise is beneficial for overall health and can help improve insulin sensitivity. However, it can also cause fluctuations in blood sugar levels. People with Type 1 diabetes should monitor their blood sugar before, during, and after exercise and adjust insulin doses or carbohydrate intake as needed. Consulting a healthcare professional before starting a new exercise regimen is advisable.
13. What is the role of insulin pumps in managing Type 1 diabetes?
Insulin pumps are small, computerized devices that deliver a steady, continuous dose of rapid-acting insulin throughout the day and can also deliver additional doses (boluses) when needed, such as during meals. They offer more precise insulin delivery compared to multiple daily injections and can help maintain stable blood sugar levels. However, they require proper training and regular monitoring.
14. Can stress affect blood sugar levels in people with Type 1 diabetes?
Yes, stress can impact blood sugar levels by triggering the release of hormones like adrenaline and cortisol, which can cause blood sugar to rise. Learning stress management techniques such as meditation, deep breathing exercises, or engaging in hobbies can help maintain better blood sugar control.
15. How can parents support a child with Type 1 diabetes?
Parents play a crucial role in helping children manage Type 1 diabetes. They should ensure that their child receives appropriate medical care, understand how to monitor blood sugar levels and provide emotional support. Educating themselves and their child about the condition, working closely with healthcare professionals, and creating a supportive home environment are essential for effective management.