Overview:
Cardiovascular disease (CVD) refers to a group of disorders affecting the heart and blood vessels, including conditions such as coronary artery disease, heart failure, arrhythmias, and stroke.
As the leading cause of death worldwide, cardiovascular disease (CVD) claims millions of lives annually.
Despite its prevalence, cardiovascular disease is often preventable through lifestyle changes, early diagnosis, and effective management.
In this blog, we will discuss what cardiovascular disease is, its symptoms, causes, risk factors, complications, diagnosis, treatment, prevention, and some frequently asked questions.
Table of Contents
What is Cardiovascular Disease?
Cardiovascular disease encompasses various heart and blood vessel conditions, such as coronary artery disease, heart attacks, strokes, and hypertension, often resulting from factors like poor diet, smoking, genetics, and lack of exercise.
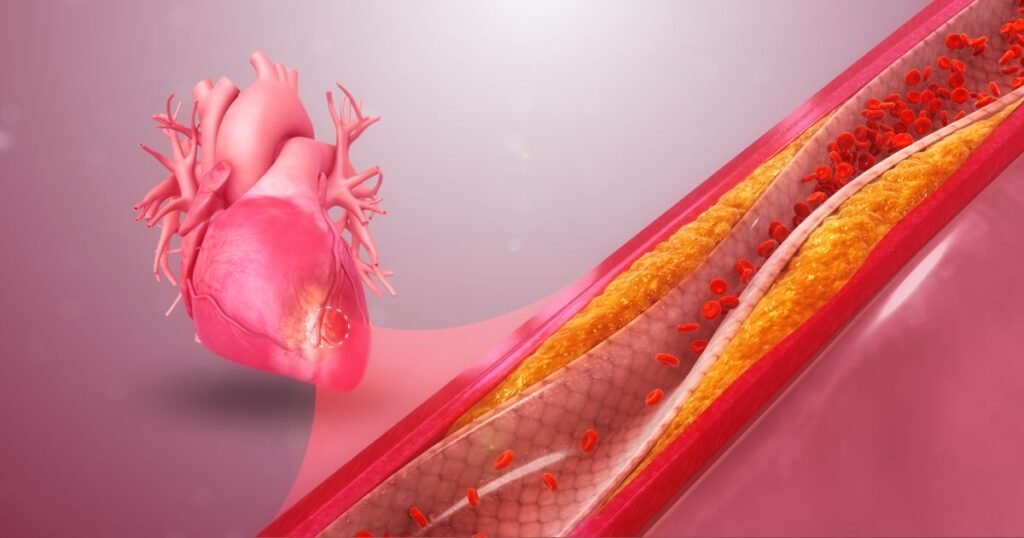
1. Coronary Artery Disease (CAD): Narrowing or blockage of the coronary arteries caused by the buildup of plaque (atherosclerosis). This can lead to chest pain (angina), heart attacks, or other complications.
2. Heart Failure: A condition in which the heart is unable to pump blood efficiently, leading to fatigue, shortness of breath, and fluid retention.
3. Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation, which can lead to palpitations, dizziness, and sometimes heart failure.
4. Stroke: This occurs when blood flow to the brain is interrupted, either by a clot (ischemic stroke) or a burst blood vessel (hemorrhagic stroke), causing brain cells to die.
5. Peripheral Artery Disease (PAD): Narrowing of the blood vessels in the limbs, particularly the legs, causing pain and mobility issues.
These conditions are often interconnected, with many patients suffering from more than one type of cardiovascular disease.
Symptoms of Cardiovascular Disease
The symptoms of cardiovascular disease vary depending on the specific condition, but common signs include:
- Chest pain or discomfort (angina): Often described as pressure, tightness, or squeezing in the chest. It may also radiate to the arms, neck, jaw, or back.
- Shortness of breath: Difficulty breathing during physical activity or even at rest may indicate heart or lung problems.
- Fatigue: Unexplained tiredness or weakness can be a symptom of heart failure or poor circulation.
- Palpitations: Feeling of irregular or fast heartbeats, which can signal arrhythmias.
- Swelling (edema): Swelling in the legs, ankles, or abdomen can be a sign of heart failure.
- Dizziness or fainting: These symptoms can occur with arrhythmias or poor blood circulation.
- Pain or discomfort in the arms, shoulders, neck, jaw, or back: This can accompany chest pain and may be more prominent in women experiencing heart attacks.
- Numbness or weakness: Sudden weakness in the face, arm, or leg, especially on one side of the body, may indicate a stroke.
It’s important to note that symptoms of cardiovascular disease can sometimes be “silent” or subtle, particularly in women. Therefore, regular checkups and attention to risk factors are crucial for early detection.
Causes of Cardiovascular Disease
Cardiovascular disease is typically caused by the buildup of plaque (a combination of fat, cholesterol, and other substances) in the arteries, a process known as atherosclerosis. This buildup leads to narrowing or hardening of the arteries, restricting blood flow to the heart and other organs. Major causes include:
- Atherosclerosis: The accumulation of plaque in the arteries, which can lead to blockages, heart attacks, and strokes.
- High blood pressure (hypertension): Uncontrolled high blood pressure damages blood vessels over time, contributing to heart disease.
- High cholesterol: Elevated levels of LDL (bad) cholesterol contribute to plaque formation in arteries.
- Smoking: Smoking damages blood vessels, reduces oxygen in the blood, and contributes to the buildup of plaque.
- Diabetes: High blood sugar levels damage blood vessels and nerves controlling the heart, significantly increasing the risk of CVD.
- Obesity: Excess body fat increases the risk of high blood pressure, high cholesterol, and diabetes, all of which are linked to heart disease.
- Sedentary lifestyle: Lack of physical activity can lead to weight gain, high blood pressure, and cholesterol imbalances, increasing the risk of CVD.
- Poor diet: Diets high in saturated fats, trans fats, sugar, and salt contribute to atherosclerosis, hypertension, and obesity.
- Alcohol consumption: Excessive alcohol intake can raise blood pressure, increase cholesterol levels, and damage the heart muscle.
- Genetic factors: A family history of cardiovascular disease increases the likelihood of developing the condition.
Risk Factors for Cardiovascular Disease
Several factors can increase the risk of developing cardiovascular disease, some of which are modifiable through lifestyle changes, while others are non-modifiable:
- Age: The risk of heart disease increases with age, particularly for men over 45 and women over 55.
- Gender: Men are generally at higher risk of heart disease at an earlier age compared to women. However, after menopause, women’s risk increases.
- Family history: A family history of heart disease or stroke increases an individual’s risk.
- Smoking: Smoking damages blood vessels and accelerates the progression of atherosclerosis.
- High blood pressure: Uncontrolled hypertension is a leading cause of heart disease and stroke.
- High cholesterol: Elevated levels of LDL cholesterol increase the risk of atherosclerosis.
- Physical inactivity: A sedentary lifestyle contributes to weight gain, high blood pressure, and cholesterol issues.
- Obesity: Excess weight strains the heart and contributes to conditions like high blood pressure and diabetes.
- Diabetes: People with diabetes are at a significantly higher risk of heart disease.
- Poor diet: Diets high in unhealthy fats, sugar, and salt can lead to high blood pressure, cholesterol issues, and obesity.
- Excessive alcohol consumption: Drinking alcohol in large quantities raises blood pressure and increases the risk of heart disease.
Complications of Cardiovascular Disease
- Heart attack: A blockage in the coronary arteries can prevent blood flow to the heart, leading to a heart attack. This can cause permanent damage to the heart muscle or be fatal.
- Heart failure: The heart may become too weak to pump blood effectively, leading to fluid buildup in the lungs, legs, and abdomen.
- Stroke: An interruption in blood flow to the brain can cause a stroke, leading to paralysis, speech difficulties, and other long-term disabilities.
- Aneurysm: A bulge in the wall of an artery can burst, causing life-threatening internal bleeding.
- Peripheral artery disease: Reduced blood flow to the limbs, particularly the legs, can lead to pain, mobility issues, or even amputation in severe cases.
- Sudden cardiac arrest: A sudden loss of heart function can occur due to arrhythmias, leading to death if not treated immediately with CPR or defibrillation.
Diagnosis of Cardiovascular Disease
Several tests and procedures are used to diagnose cardiovascular disease:
- Blood tests: To check for high cholesterol, blood sugar levels (diabetes), and markers of heart damage (like troponin).
- Electrocardiogram (ECG): A test that records the electrical activity of the heart and detects irregular heart rhythms or heart attacks.
- Echocardiogram: An ultrasound of the heart that provides images of the heart’s structure and function.
- Stress test: Involves exercising on a treadmill or bike while monitoring heart activity to detect issues with blood flow.
- Coronary angiography: A special dye is injected into the bloodstream to highlight blockages in the coronary arteries on X-ray images.
- CT or MRI scans: These imaging tests provide detailed pictures of the heart and blood vessels to identify abnormalities.
Treatment of Cardiovascular Disease
Treatment for cardiovascular disease often involves a combination of lifestyle changes, medications, and in some cases, surgery. Common treatments include:
1. Lifestyle changes:
- Quitting smoking
- Eating a heart-healthy diet (low in saturated fats, salt, and sugar)
- Exercising regularly (at least 30 minutes of moderate activity most days of the week)
- Maintaining a healthy weight
- Reducing alcohol intake
2. Medications:
- Blood pressure medications: Such as ACE inhibitors, beta-blockers, or diuretics to lower blood pressure.
- Cholesterol-lowering drugs: Statins are commonly prescribed to lower LDL cholesterol and reduce the risk of heart attacks and strokes.
- Anticoagulants (blood thinners): Such as aspirin or warfarin, to reduce the risk of blood clots.
- Beta-blockers: Help reduce heart rate and blood pressure, relieving stress on the heart.
3. Surgical procedures:
- Angioplasty and stent placement: Involves inserting a balloon catheter to open up blocked arteries and placing a stent to keep the artery open.
- Coronary artery bypass surgery: In severe cases of coronary artery disease, a surgeon may reroute blood flow around blocked arteries using grafts from other blood vessels.
- Pacemaker or defibrillator: Devices implanted to help regulate abnormal heart rhythms.
Prevention of Cardiovascular Disease
Preventing cardiovascular disease involves adopting heart-healthy habits that reduce the risk of plaque buildup and other risk factors:
- Quit smoking: Smoking is one of the most significant risk factors for cardiovascular disease. Quitting can rapidly reduce the risk of heart attacks and strokes.
- Healthy diet: Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats like those found in dairy products, nuts, and olive oil. Limit processed foods, and salt.
- Exercise regularly: Aim for at least 150 minutes of moderate exercise each week to maintain a healthy weight, reduce blood pressure, and improve heart function.
- Maintain a healthy weight: Losing even a small amount of weight can lower blood pressure, cholesterol levels, and the risk of diabetes.
- Avoid alcohol: Avoiding alcohol prevents the risk of cardiovascular diseases. According to WHO, there is no safe amount of alcohol that does not affect health.
- Manage stress: Chronic stress can contribute to high blood pressure and heart disease. Practice stress-reducing techniques such as meditation, yoga, or deep breathing exercises.
- Regular checkups: Monitor blood pressure, cholesterol levels, and blood sugar regularly, and follow your healthcare provider’s advice for managing any health conditions.
Conclusion
Cardiovascular disease is a widespread and serious condition, but it is often preventable through healthy lifestyle choices and early intervention.
By recognizing the risk factors, symptoms, and complications, individuals can take proactive steps to protect their heart health.
Whether through lifestyle modifications, medications, or surgical interventions, managing cardiovascular disease requires a comprehensive approach involving healthcare professionals and personal commitment.
Early diagnosis and effective treatment can greatly improve the quality of life for those affected by CVD and reduce the risk of life-threatening complications like heart attacks, strokes, and heart failure.
Being heart-conscious in our everyday lives—whether by staying active, eating right, or reducing stress—can make all the difference in preventing cardiovascular disease.
FAQs:
1. Can cardiovascular disease be cured?
There is no cure for cardiovascular disease, but it can be managed effectively with lifestyle changes, medications, and sometimes surgery. Early intervention and proper treatment can significantly improve the quality of life and reduce complications.
2. What is the difference between a heart attack and a stroke?
A heart attack occurs when blood flow to the heart is blocked, usually by a clot or plaque buildup. A stroke happens when blood flow to the brain is interrupted, either by a clot (ischemic stroke) or bleeding (hemorrhagic stroke).
3. Is high cholesterol always a cause of cardiovascular disease?
High cholesterol, especially LDL (bad) cholesterol, is a major risk factor for cardiovascular disease. However, it’s just one of many factors. A healthy lifestyle can lower cholesterol and reduce heart disease risk.
4. How can I lower my risk of heart disease if it runs in my family?
Even if you have a family history of heart disease, you can reduce your risk by not smoking, eating a healthy diet, exercising regularly, managing stress, and keeping your blood pressure, cholesterol, and blood sugar levels under control.
5. Are women at lower risk for cardiovascular disease than men?
While men tend to develop heart disease earlier than women, the risk for women increases after menopause. Cardiovascular disease is the leading cause of death for women, making it just as critical to manage risk factors.

