Overview
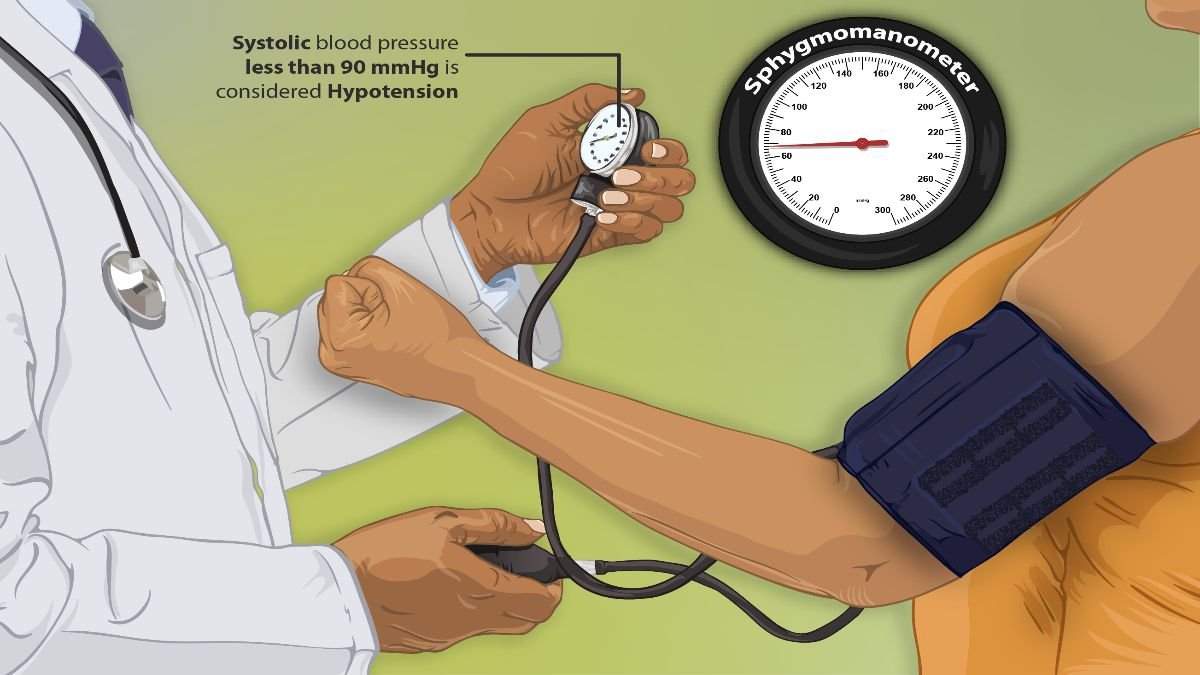
Low blood pressure, also known as hypotension, occurs when blood pressure readings fall below the normal range, usually less than 90 mm Hg systolic or 60 mm Hg diastolic.
While high blood pressure (hypertension) is often more commonly discussed, low blood pressure can also cause significant health issues.
For many, hypotension may not cause noticeable symptoms, but in others, it can lead to dizziness, fainting, and even shock in severe cases.
In this blog, we will delve into the causes, symptoms, risk factors, complications, diagnosis, treatment, and prevention of low blood pressure, providing helpful tips to manage this condition effectively.
Table of Contents
What is Low Blood Pressure?

Blood pressure is the force exerted by circulating blood on the walls of blood vessels. A blood pressure reading consists of two numbers: the systolic pressure (the first number) measures the pressure in the arteries when the heart beats, and the diastolic pressure (the second number) measures the pressure in the arteries between beats.
Generally, a blood pressure reading lower than 90/60 mm Hg is considered low, although the threshold for concern varies by individual.
For some people, low blood pressure is a natural state and does not cause any symptoms. However, for others, it may signal an underlying health condition or lead to inadequate blood flow to vital organs, especially the brain, heart, and kidneys.
Symptoms of Low Blood Pressure
While low blood pressure might not always cause symptoms, when it does, these can include:
- Dizziness or lightheadedness
- Fainting (syncope)
- Blurred or impaired vision
- Nausea
- Fatigue or weakness
- Rapid, shallow breathing
- Confusion or difficulty concentrating
Symptoms often occur or worsen when standing up suddenly or after prolonged periods of standing, a condition known as orthostatic hypotension.
Causes of Low Blood Pressure
Several factors can contribute to low blood pressure, and understanding the root cause is essential for proper management. Some common causes include:
- Dehydration: When the body loses more water than it takes in, blood volume decreases, leading to a drop in blood pressure.
- Heart problems: Conditions like bradycardia (slow heart rate), heart valve problems, heart attack, and heart failure can lead to low blood pressure due to impaired heart function.
- Endocrine disorders: Hormonal imbalances, including adrenal insufficiency (Addison’s disease), low blood sugar (hypoglycemia), and certain thyroid conditions, can lower blood pressure.
- Severe infection (septicemia): A bloodstream infection can lead to a dangerous drop in blood pressure, a condition called septic shock.
- Blood loss: Significant blood loss from trauma, surgery, or internal bleeding can lead to low blood pressure as blood volume decreases.
- Nutritional deficiencies: A lack of essential nutrients, particularly vitamin B12 and folate, can prevent the body from producing enough red blood cells, leading to low blood pressure.
- Medications: Certain medications, including diuretics, beta-blockers, antidepressants, and drugs for Parkinson’s disease, can lower blood pressure.
- Pregnancy: Blood pressure naturally decreases during pregnancy, especially in the first and second trimesters, due to hormonal changes and increased blood volume.
- Orthostatic hypotension: A sudden drop in blood pressure when changing positions (such as standing up quickly) can cause dizziness or fainting.
- Postprandial hypotension: This occurs after eating and is more common in older adults, as blood flow is redirected to the digestive system, which may cause a temporary drop in blood pressure.
Risk Factors for Low Blood Pressure
Certain factors increase the likelihood of experiencing low blood pressure, including:
- Age: Low blood pressure upon standing or after eating primarily affects older adults, particularly those over 65.
- Medications: Using certain drugs to treat high blood pressure, depression, or Parkinson’s disease can lead to hypotension.
- Pre-existing conditions: Diseases like diabetes, Parkinson’s disease, and certain heart conditions increase the risk of low blood pressure.
- Dehydration: Those with a history of dehydration or electrolyte imbalances are more susceptible to hypotension.
Complications of Low Blood Pressure
When blood pressure remains consistently low, it can lead to complications that affect the quality of life and even increase health risks:
- Falls and injuries: Hypotension-related dizziness or fainting increases the likelihood of falls, which can lead to injuries.
- Shock: In severe cases, low blood pressure can cause shock, a life-threatening condition where vital organs do not receive enough oxygen and nutrients.
- Organ damage: Chronic low blood pressure can impact blood flow to critical organs, potentially leading to issues in the heart, kidneys, and brain.
- Increased fall risk in older adults: Orthostatic hypotension is common in older adults and can lead to frequent falls, posing a risk to bone health.
Diagnosis of Low Blood Pressure
To diagnose low blood pressure, doctors will first conduct a physical exam and review medical history. Additional tests may include:
- Blood pressure measurements: Multiple readings are often taken, especially after standing, sitting, and lying down, to observe fluctuations in blood pressure.
- Blood tests: These help identify underlying causes like anemia, low blood sugar, or electrolyte imbalances.
- Electrocardiogram (ECG): An ECG is used to check for any irregular heart rhythms or other heart-related issues.
- Echocardiogram: This ultrasound test of the heart allows doctors to observe heart function and identify structural issues.
- Tilt table test: This test helps diagnose orthostatic hypotension by monitoring blood pressure and heart rate as the table tilts to simulate changing positions.
Treatment of Low Blood Pressure
Treatment for low blood pressure depends on the underlying cause and severity of symptoms. Options may include:
Lifestyle Changes
- Increase salt intake (under medical supervision): Salt can raise blood pressure, so individuals with hypotension may benefit from a slightly higher salt intake, although this must be monitored by a healthcare provider.
- Stay hydrated: Drinking plenty of water increases blood volume, which can help maintain stable blood pressure.
- Wear compression stockings: These can help reduce blood pooling in the legs and improve circulation.
- Eat smaller, more frequent meals: For those experiencing postprandial hypotension, smaller meals can help prevent sudden drops in blood pressure after eating.
- Move slowly when changing positions: Standing up gradually after sitting or lying down can prevent dizziness caused by orthostatic hypotension.
Medications
For more severe cases, medications may be prescribed to raise blood pressure:
- Fludrocortisone: This medication helps increase blood volume, which can improve blood pressure.
- Midodrine: Midodrine is often used to treat orthostatic hypotension as it helps constrict blood vessels, thereby raising blood pressure.
- Erythropoietin: For patients with anemia-related hypotension, erythropoietin may be prescribed to stimulate red blood cell production and boost blood pressure.
Prevention of Low Blood Pressure
Although it may not always be possible to prevent low blood pressure, certain practices can help reduce its occurrence:
- Drink fluids regularly: Proper hydration can prevent dehydration, a major contributor to hypotension.
- Avoid alcohol consumption: Alcohol can lead to dehydration and lower blood pressure, so avoid it.
- Avoid prolonged bed rest: Staying active helps maintain normal blood pressure levels.
- Eat a balanced diet: A diet rich in nutrients, particularly vitamins B12 and folate, supports healthy blood pressure.
- Monitor your blood pressure regularly: Keeping track of blood pressure helps you recognize any unusual drops and allows for early intervention if needed.
Conclusion
Low blood pressure, while often less discussed than high blood pressure, can lead to discomfort and health risks if not managed properly.
By understanding the symptoms, causes, and treatments for hypotension, you can better manage or prevent this condition.
If you experience symptoms of low blood pressure, consult a healthcare professional for a proper diagnosis and treatment plan tailored to your needs.
Frequently Asked Questions (FAQs)
1. What foods can help raise low blood pressure?
Salted foods, caffeine (in moderation), and foods rich in B vitamins can support healthy blood pressure. Always consult your healthcare provider about dietary changes.
2. Is low blood pressure always a concern?
No, low blood pressure is not always a concern. For some people, it’s normal and doesn’t cause symptoms. However, if it leads to dizziness, fainting, or shock, it should be addressed.
3. Can exercise improve low blood pressure?
Yes, regular exercise helps improve blood circulation and can raise blood pressure. However, exercise should be done under medical guidance if you have hypotension.
4. Are there long-term complications associated with low blood pressure?
Untreated chronic low blood pressure can lead to complications such as falls, fainting, or damage to organs due to inadequate blood flow.
5. When should I see a doctor for low blood pressure?
If you experience frequent dizziness, fainting, confusion, or other symptoms that interfere with daily life, see a doctor to identify any underlying causes and receive appropriate treatment.
6. How is low blood pressure diagnosed?
Diagnosis typically involves measuring blood pressure, reviewing medical history, and performing tests to identify underlying conditions.
7. What are the treatments for low blood pressure?
Treatment may include lifestyle changes, increased salt intake, hydration, medications, or addressing underlying conditions.
8. How can I manage low blood pressure at home?
Staying hydrated, wearing compression stockings, avoiding alcohol, and eating small, frequent meals can help manage low blood pressure.
9. Are there any lifestyle changes that can help?
Yes, maintaining a healthy diet, regular exercise, and managing stress can improve overall cardiovascular health and help stabilize blood pressure.
10. Is low blood pressure more common in certain age groups?
Hypotension can occur in any age group, but it is more common in older adults due to age-related changes in the cardiovascular system.