Overview:
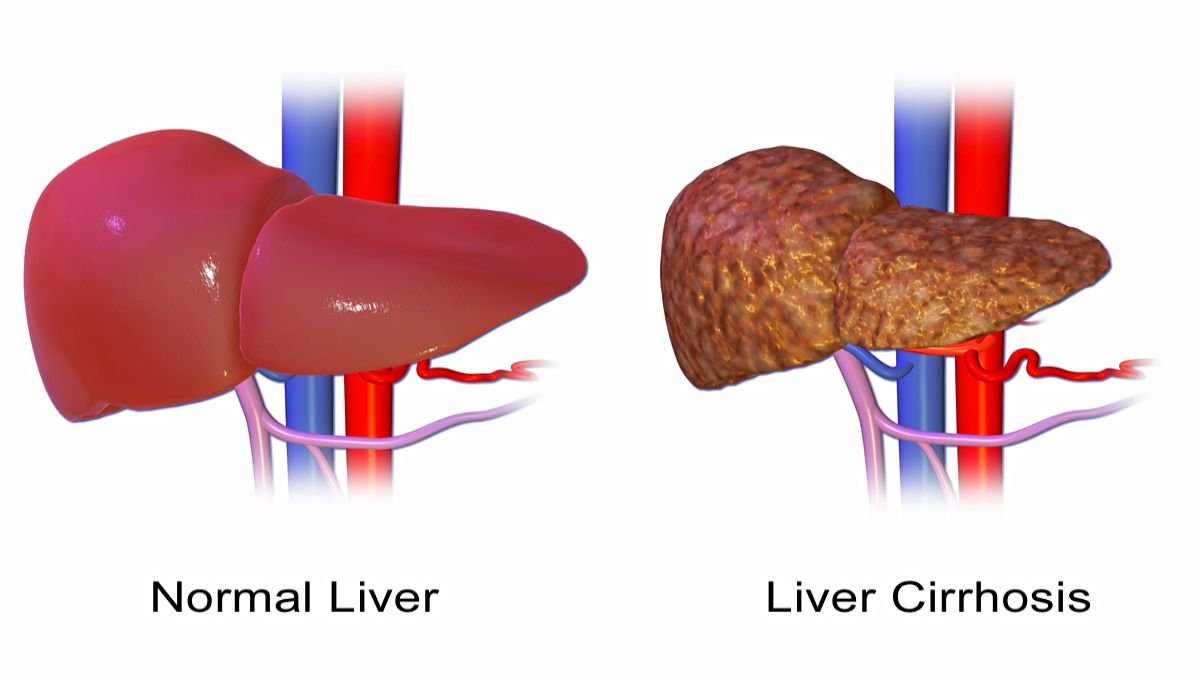
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, and end-stage liver disease, is a late-stage liver disease that results from chronic liver damage.
It is characterized by the replacement of healthy liver tissue with scar tissue, leading to impaired liver function.
The liver is capable of regenerating itself, but repeated damage—whether from infections, toxins, or other diseases, leads to the accumulation of scar tissues.
Once scar tissue forms, it blocks the normal flow of blood through the liver and impairs the liver’s ability to perform its vital functions, such as detoxification, protein production, and nutrient storage.
In this blog, we will explore the symptoms, causes, risk factors, complications, diagnosis, treatment, and prevention of cirrhosis.
We will also provide a comprehensive overview to help you understand the importance of liver health and how to manage and prevent this chronic condition.
Table of Contents
What Is Cirrhosis?
Cirrhosis is a progressive condition that occurs as a result of long-term liver damage. The liver, a vital organ responsible for numerous essential functions, becomes scarred and hardened due to continuous injury from various factors.
This scarring interferes with the liver’s ability to function properly, leading to potentially life-threatening complications.
As the scar tissue increases, the liver becomes increasingly dysfunctional, and cirrhosis progresses. If left untreated, cirrhosis can lead to liver failure, liver cancer, and death.
Symptoms of Cirrhosis
Cirrhosis often does not cause symptoms in its early stages. As the disease progresses, symptoms become more noticeable and severe. Common symptoms of cirrhosis include:
- Fatigue: A general feeling of tiredness or lack of energy is common in people with cirrhosis.
- Jaundice: Yellowing of the skin and eyes due to the accumulation of bilirubin, a waste product that the liver is unable to process effectively.
- Easy Bruising and Bleeding: The liver’s decreased ability to produce clotting factors leads to easy bruising and frequent bleeding.
- Swelling (Edema): Fluid may accumulate in the legs (edema) and abdomen (ascites), causing swelling and discomfort.
- Loss of Appetite and Weight Loss: People with cirrhosis may lose their appetite, leading to unintentional weight loss and malnutrition.
- Nausea and Vomiting: Persistent nausea and vomiting can occur, especially as the liver becomes more damaged.
- Spider Angiomas: Small, spider-like blood vessels may appear on the skin.
- Itchy Skin: Bile salts that accumulate in the bloodstream due to liver dysfunction can cause intense itching.
- Confusion and Difficulty Thinking: As cirrhosis progresses, toxins that the liver would normally filter out can accumulate in the brain, leading to confusion, memory problems, and difficulty concentrating.
Causes of Cirrhosis
Cirrhosis can develop from a variety of causes, with chronic liver diseases and long-term liver damage being the most common culprits. Some of the leading causes of cirrhosis include:
- Chronic Alcohol Abuse: Excessive alcohol consumption over many years is a major cause of cirrhosis, as it leads to repeated liver inflammation and damage.
- Chronic Viral Hepatitis (Hepatitis B and C): Long-term infection with hepatitis B or C can cause liver inflammation, which eventually leads to cirrhosis.
- Non-Alcoholic Fatty Liver Disease (NAFLD): This condition occurs when fat accumulates in the liver, causing inflammation and damage. It is closely associated with obesity, type 2 diabetes, and metabolic syndrome.
- Autoimmune Hepatitis: In this condition, the body’s immune system attacks liver cells, causing chronic inflammation and liver damage.
- Genetic Disorders: Certain genetic conditions, such as hemochromatosis (excess iron buildup in the liver) and Wilson’s disease (excess copper buildup), can lead to cirrhosis.
- Bile Duct Disorders: Conditions that affect the bile ducts, such as primary biliary cholangitis or primary sclerosing cholangitis, can lead to cirrhosis by blocking the flow of bile, causing liver damage.
- Prolonged Exposure to Toxins: Long-term exposure to environmental toxins or certain medications can also cause liver damage and lead to cirrhosis.
Risk Factors for Cirrhosis
Certain risk factors increase the likelihood of developing cirrhosis. Some of the most significant risk factors include:
- Chronic Alcoholism: Heavy drinking over many years is a leading risk factor for cirrhosis.
- Chronic Viral Hepatitis: Individuals with long-term hepatitis B or C infections are at higher risk of developing cirrhosis.
- Obesity: Being overweight or obese increases the risk of developing non-alcoholic fatty liver disease, which can progress to cirrhosis.
- Diabetes: People with type 2 diabetes are more prone to liver disease, including NAFLD and cirrhosis.
- Genetic Liver Diseases: Inherited conditions such as hemochromatosis or Wilson’s disease increase the risk of cirrhosis.
- Long-Term Medication Use: Chronic use of certain medications can lead to liver damage and cirrhosis over time.
- Exposure to Toxins: Long-term exposure to environmental toxins or chemicals can increase the risk of liver damage and cirrhosis.
Complications of Cirrhosis
Cirrhosis can lead to a range of serious complications, many of which are life-threatening. These include:
- Liver Failure: As liver function continues to decline, the liver may lose its ability to perform essential tasks, leading to liver failure.
- Portal Hypertension: Scar tissue in the liver obstructs blood flow, leading to increased pressure in the portal vein, which can cause varices (enlarged veins) and bleeding.
- Ascites: Accumulation of fluid in the abdomen due to increased pressure in the blood vessels and impaired liver function.
- Hepatic Encephalopathy: A buildup of toxins in the brain, leading to confusion, disorientation, and changes in behavior.
- Kidney Failure: Cirrhosis can cause kidney dysfunction, leading to a condition called hepatorenal syndrome, which is life-threatening.
- Infections: People with cirrhosis are at higher risk for infections, especially spontaneous bacterial peritonitis, which occurs in the fluid that accumulates in the abdomen (ascites).
- Liver Cancer: Cirrhosis increases the risk of developing hepatocellular carcinoma, the most common form of liver cancer.
Diagnosis of Cirrhosis
Cirrhosis is typically diagnosed through a combination of medical history, physical examination, blood tests, imaging studies, and sometimes a liver biopsy. Common diagnostic methods include:
- Blood Tests: These tests can check liver function and detect abnormalities in liver enzymes, bilirubin levels, and blood clotting factors.
- Imaging Tests: Ultrasound, CT scans, or MRI can provide images of the liver and reveal signs of cirrhosis, such as scarring or enlargement.
- Liver Biopsy: In some cases, a liver biopsy may be performed to confirm the diagnosis and assess the extent of liver damage.
- Elastography: This non-invasive imaging test measures liver stiffness, which can indicate the presence and severity of fibrosis (scarring).
Treatment of Cirrhosis
While cirrhosis cannot be reversed, treatment focuses on managing symptoms, slowing disease progression, and preventing complications. Treatment options may include:
- Lifestyle Changes: Quitting alcohol is crucial for people with alcohol-related cirrhosis. Maintaining a healthy weight and managing underlying conditions like diabetes and high cholesterol are also important.
- Medications: Medications may be prescribed to treat the underlying cause of cirrhosis (e.g., antiviral drugs for hepatitis B or C) or to manage complications like portal hypertension and hepatic encephalopathy.
- Nutritional Support: People with cirrhosis often require a special diet, as malnutrition is common. A diet rich in protein, vitamins, and minerals is recommended to support liver function.
- Management of Complications: Specific treatments may be required to manage complications, such as diuretics for ascites, antibiotics for infections, and beta-blockers to reduce the risk of variceal bleeding.
- Liver Transplant: For advanced cirrhosis or liver failure, a liver transplant may be the only option. A liver transplant can replace the damaged liver with a healthy donor liver and provide a cure for cirrhosis.
Prevention of Cirrhosis
Preventing cirrhosis involves protecting the liver from damage by addressing the underlying causes of liver disease. Key preventive measures include:
- Avoid Alcohol: Avoiding alcohol consumption is essential for reducing the risk of liver damage and cirrhosis.
- Vaccination: Vaccination against hepatitis B can prevent infection and reduce the risk of cirrhosis. People at high risk of hepatitis C should take precautions to avoid infection.
- Healthy Diet and Exercise: Maintaining a healthy weight through diet and regular exercise can help prevent non-alcoholic fatty liver disease and cirrhosis.
- Avoid Toxins: Limiting exposure to environmental toxins, harmful chemicals, and certain medications can reduce the risk of liver damage.
- Regular Check-ups: Regular medical check-ups and liver function tests can help identify liver problems early and prevent further damage. This is especially important for individuals with risk factors such as chronic alcohol use, viral hepatitis, or metabolic disorders.
- Manage Underlying Health Conditions: Proper management of conditions like diabetes, obesity, and high cholesterol can reduce the risk of developing cirrhosis, especially in individuals prone to non-alcoholic fatty liver disease.
Conclusion
Cirrhosis is a serious and potentially life-threatening condition that results from long-term liver damage. While the liver is a resilient organ, repeated injury can lead to the accumulation of scar tissue, impairing its function and causing complications.
Recognizing the symptoms early, understanding the underlying causes, and making lifestyle changes are essential to managing and preventing cirrhosis.
Treatment focuses on slowing the progression of the disease, managing complications, and, in severe cases, liver transplantation may be necessary.
Preventive measures such as limiting alcohol consumption, maintaining a healthy weight, getting vaccinated for hepatitis, and managing underlying health conditions are crucial to protect liver health.
With early diagnosis and appropriate management, the progression of cirrhosis can be slowed, improving the quality of life for those affected.
Frequently Asked Questions (FAQs)
1. Can cirrhosis be cured?
Cirrhosis cannot be completely cured, as the damage caused by scarring in the liver is irreversible. However, with early diagnosis and proper treatment, the progression of cirrhosis can be slowed, and its complications can be managed. In cases of advanced cirrhosis, liver transplantation may offer a chance for a cure.
2. Is cirrhosis always caused by alcohol consumption?
No, cirrhosis can result from a variety of causes. While chronic alcohol consumption is a leading cause, viral hepatitis (especially hepatitis B and C), non-alcoholic fatty liver disease, genetic disorders, and autoimmune diseases can also lead to cirrhosis.
3. How long can a person live with cirrhosis?
The prognosis for someone with cirrhosis depends on the stage of the disease, the underlying cause, and how well the condition is managed. With early diagnosis and proper management, individuals with cirrhosis can live for many years. However, advanced cirrhosis or liver failure can significantly shorten life expectancy if not treated.
4. What are the early signs of cirrhosis?
In the early stages, cirrhosis may not cause noticeable symptoms. As the disease progresses, common symptoms include fatigue, jaundice (yellowing of the skin and eyes), easy bruising, swelling in the legs and abdomen, loss of appetite, and nausea.
5. Can cirrhosis lead to liver cancer?
Yes, cirrhosis increases the risk of developing liver cancer, particularly hepatocellular carcinoma (HCC). Regular screening and monitoring for liver cancer are recommended for individuals with cirrhosis.
6. How is cirrhosis diagnosed?
Cirrhosis is diagnosed through a combination of medical history, physical examination, blood tests, imaging studies (such as ultrasound, CT scan, or MRI), and sometimes a liver biopsy. Elastography, a non-invasive test that measures liver stiffness, is also commonly used to assess fibrosis.
7. What foods should be avoided with cirrhosis?
People with cirrhosis should avoid alcohol entirely. Additionally, it is important to limit salty and fatty foods, as these can contribute to fluid retention (ascites) and fatty liver disease. A healthy, balanced diet rich in fruits, vegetables, lean proteins, and whole grains is recommended.
8. Is liver transplantation the only treatment option for advanced cirrhosis?
For individuals with advanced cirrhosis or liver failure, liver transplantation may be the only option. However, for those with early-stage cirrhosis, lifestyle changes, medications, and managing complications can help slow the progression of the disease and improve quality of life.
9. Can cirrhosis be prevented?
Yes, cirrhosis can often be prevented by avoiding risk factors such as alcohol consumption, preventing hepatitis infections through vaccination, maintaining a healthy weight, and managing underlying health conditions like diabetes and obesity.
10. Can cirrhosis be reversed if caught early?
While cirrhosis cannot be reversed, catching the disease in its early stages allows for better management and can prevent further liver damage. Early intervention, including lifestyle changes and treatment of the underlying cause, can slow the progression of the disease and improve outcomes.