What is type 2 diabetes?
Type 2 diabetes is a chronic medical condition that occurs when your body becomes resistant to insulin or doesn’t produce enough insulin to maintain normal sugar(glucose) levels. It causes high levels of sugar in your bloodstream.
Insulin is a hormone released by the pancreas gland situated in your liver that is responsible for the movement of sugar(glucose) from your blood to your body’s cells. Your body’s cells use glucose to produce energy to do work.
However, with type 2 diabetes, your body’s cells don’t respond to insulin as effectively as in normal conditions. It causes your body’s cells to take in less sugar from your blood thus leading to accumulation or build-up of sugar in your blood.
In the later stages of the condition, it can damage your pancreas and your body may not produce enough insulin.
High blood sugar can lead to several health complications like circulatory, nervous, and immune system disorders.
Table of Contents
Types Of Diabetes:
There are three main types of diabetes:
- Type 1 Diabetes: In type 1 diabetes, your immune system mistakenly attacks and destroys the beta cells in your pancreas that produce insulin. This damage is permanent and your body will not produce any insulin. 5 to 10% of people with diabetes have type 1 diabetes.
- Type 2 Diabetes: In type 2 diabetes, your body’s cells become less responsive to insulin. 90 to 95% of people with diabetes have type 2 diabetes.
- Gestational diabetes: This type of diabetes only develops during pregnancy. It usually goes away after giving birth.
Symptoms of type 2 diabetes:
Symptoms of type 2 diabetes often develop slowly and even you can’t notice them for many years.
- Excessive thirst
- Constant hunger
- A lack of energy
- Frequent urination
- Blurred vision
- Fatigue
- Weight loss without trying
- Getting infections frequently
- Wounds that don’t heal
- Dark rashes around your neck or armpits
- Numbness or tingling in the hands or feet
When the disease enters into later stages, symptoms become more severe and can cause some potentially dangerous complications including:
- Eye problems (diabetic retinopathy)
- Kidney disease (nephropathy)
- Heart attack or stroke
- Gum disease
- Feelings of numbness in your extremities, or neuropathy
Causes of type 2 diabetes:
- Genetics: A family history of diabetes increases the risk significantly. Certain genetic mutations can affect how your body produces or utilizes insulin.
- Insulin resistance: When your body’s cells become resistant to the action of insulin, leading to high levels of sugar in your bloodstream.
- Obesity: Excess body fat, especially around the abdomen, increases the risk of insulin resistance.
- Unhealthy diet: Ultra-processed foods that are high in added sugars, unhealthy fats, and low in fiber can contribute to insulin resistance and obesity.
- Physical inactivity: Lack of exercise reduces the body’s ability to regulate blood sugar levels and utilize insulin effectively.
- Damaged pancreas: The damaged pancreas cannot produce enough insulin to maintain normal glucose levels in your body.
- Age: The risk of developing type 2 diabetes increases after you turn 45 years old.
- Ethnicity: Some ethnic groups such as African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans have a higher risk of developing type 2 diabetes.
- Gestational diabetes: Women with gestational diabetes during pregnancy have a higher risk of developing type 2 diabetes later in life.
- Certain medical conditions: Certain medical conditions such as high blood pressure, polycystic ovary syndrome (PCOS), and sleep disorders like sleep apnea can lead to diabetes.
Diagnosis of type 2 diabetes:
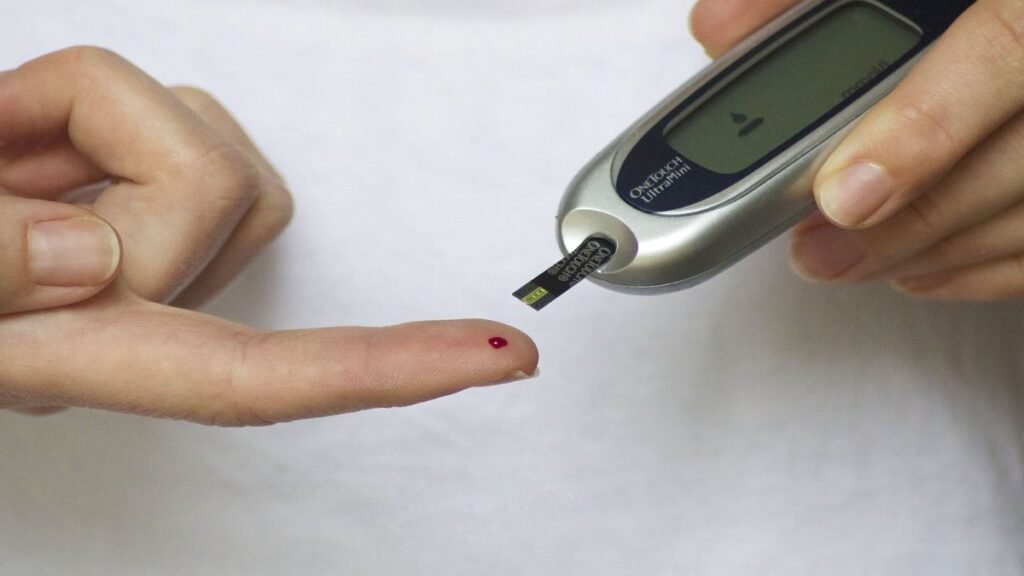
Your doctor can find out whether you have diabetes or not by testing your blood. Diagnosing testing includes:
- Hemoglobin A1C test: This test measures your average blood sugar levels for the past 2 or 3 months.
- Fasting plasma glucose test: It measures your blood sugar(glucose) level on an empty stomach. You won’t be able to eat or drink anything except water for 8 hours before the test.
- Oral glucose tolerance test: This test checks your blood glucose level before and after 2 hours you drink something sweet to see how your body deals with the glucose before and after you drink.
Treatment of type 2 diabetes:
Type 2 diabetes can be managed, and in some cases, reversed. Keeping your blood sugar level, blood pressure, and cholesterol within a healthy range is essential to manage your type 2 diabetes. In some cases, you need medication.
Lifestyle changes that play a crucial role in managing your type 2 diabetes include:
- Healthy Diet: Incorporating a healthy diet including fruits, vegetables, and whole grains that are rich in fiber, healthy fats, and carbs can help you keep your blood sugar levels normal.
- Losing weight: Losing weight is an important factor in managing your diabetes. Losing 5% of your body weight can change your blood sugar level.
- Exercise: 30 to 60 minutes of daily physical exercise helps manage your diabetes. It keeps your glucose level, blood pressure, and cholesterol within a healthy range.
However, in some cases, if you are not able to maintain your sugar level by lifestyle changes you need medication. Not every patient needs to take insulin.
Complications linked with type 2 diabetes:
A good diabetes care plan can help protect against many diabetes-related problems. However, if not properly managed, diabetes can lead to serious complications, including:
- Cardiovascular diseases like heart attack, stroke, and high blood pressure.
- Nerve damage (neuropathy)
- Kidney damage (nephropathy)
- Eye damage, retinal damage (retinopathy)
- Sexual and bladder problems
- Skin diseases
- Foot problems
- Gum disease and other dental problems
Prevention:
Adopting a healthy lifestyle can reduce your chances of developing type 2 diabetes. Here are some things that you can do to lower your risks:
- Weight loss: If you are overweight, losing just 5 to 7% of your body weight can lower or prevent your risk of getting type 2 diabetes.
- Physical activity: Exercise for at least 30 minutes a day can help you prevent type 2 diabetes.
- Healthy meals: Eat nutritious foods that are rich in fiber, minerals, vitamins, healthy fats, and healthy carbs. Avoid highly processed foods such as soda, carbonated drinks, and fast food that are high in refined sugar, fats, salts, food colors, and preservatives.
The Bottom Line:
Managing type 2 diabetes requires a multifaceted approach that includes lifestyle changes, medication adherence( in severe cases), and regular monitoring.
By adopting healthy habits such as maintaining a balanced diet, engaging in regular physical activity, and staying informed about your condition, you can significantly improve your quality of life and reduce the risk of complications.
Remember, diabetes management is a journey that requires commitment and perseverance, but with the right support and knowledge, you can successfully navigate it and lead a fulfilling life.