Overview:
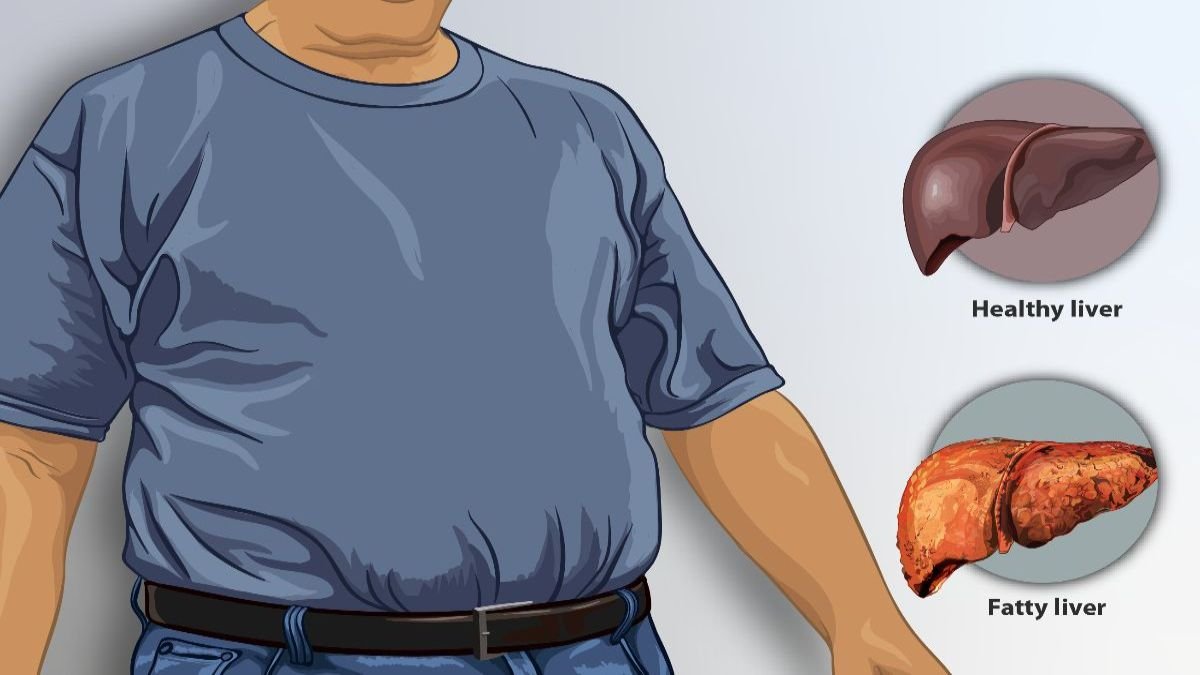
Non-alcoholic fatty liver disease (NAFLD) is rapidly becoming a prevalent health concern worldwide. It refers to a range of liver conditions that affect individuals who drink little to no alcohol.
The hallmark of NAFLD is the accumulation of excess fat in the liver, which can lead to serious complications if not managed properly.
NAFLD is often referred to as a “silent” liver condition because many individuals experience no symptoms until the disease has progressed significantly.
This blog delves into what NAFLD is, its symptoms, causes, risk factors, complications, treatment options, and preventive measures, offering a comprehensive overview of this growing health issue.
Table of Contents
What is Non-Alcoholic Fatty Liver Disease (NAFLD)?
Non-alcoholic fatty liver disease is a condition in which excess fats build up in the liver.
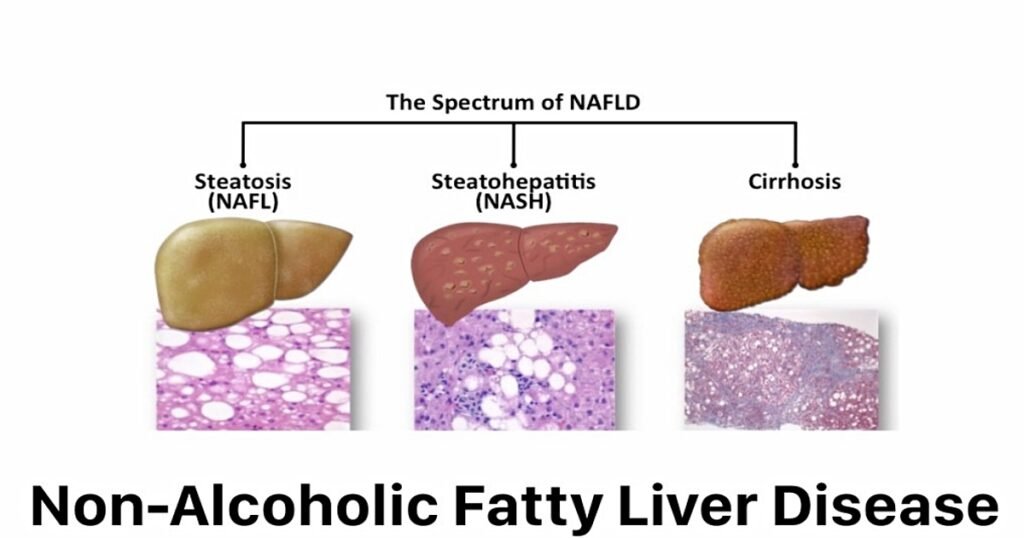
NAFLD encompasses a spectrum of liver conditions, ranging from simple fatty liver (steatosis) to non-alcoholic steatohepatitis (NASH), which can lead to cirrhosis or liver cancer.
It occurs when more than 5% of the liver’s weight is made up of fat. Unlike alcoholic liver disease, NAFLD occurs in people who drink little or no alcohol. There are two main types:
- Simple Fatty Liver (Steatosis): This form of NAFLD involves fat accumulation in the liver without significant inflammation or liver cell damage. It is generally considered a benign condition but can progress to more serious stages.
- Non-Alcoholic Steatohepatitis (NASH): NASH is a more severe form of NAFLD that involves inflammation and liver cell damage in addition to fat accumulation. It can progress to scarring (fibrosis), cirrhosis, and even liver cancer. About 20% of people with NAFLD suffer from NASH.
Symptoms of NAFLD
In its early stages, NAFLD often presents no symptoms, making it difficult to detect without medical tests. However, as the disease progresses, some individuals may experience:
- Fatigue: A general feeling of tiredness or lack of energy.
- Abdominal Discomfort: Pain or discomfort in the upper right side of the abdomen, where the liver is located.
- Nausea: Feeling sick or having an upset stomach.
- Unexplained Weight Loss: Sudden or gradual weight loss not associated with diet or exercise.
- Enlarged Liver (Hepatomegaly): This may be detected during a physical exam or imaging tests.
- Jaundice: In advanced stages, yellowing of the skin and eyes may occur due to liver damage.
Causes of NAFLD
The exact cause of non-alcoholic fatty liver disease (NAFLD) is not fully understood, but several factors contribute to the development of the condition:
- Insulin Resistance: When cells become resistant to insulin, the body produces more of the hormone, which can lead to fat buildup in the liver.
- Metabolic Syndrome: Conditions such as obesity, high blood pressure, high cholesterol, and type 2 diabetes increase the likelihood of developing NAFLD.
- High Fat Diet: Diets high in saturated fats, sugars, and refined carbohydrates can lead to liver fat accumulation.
- Genetics: Genetic predisposition may play a role in how fat is processed and stored in the liver.
- Certain medications: Some drugs can lead to liver fat accumulation.
Risk Factors for NAFLD
Several risk factors increase the likelihood of developing NAFLD, including:
- Obesity: Excess body weight is one of the most significant risk factors for NAFLD, especially abdominal or visceral fat.
- Type 2 Diabetes: Individuals with diabetes are at higher risk of developing fatty liver disease due to insulin resistance.
- High Cholesterol and Triglycerides: Elevated levels of fat in the blood can lead to fat accumulation in the liver.
- Metabolic Syndrome: A combination of conditions, including obesity, insulin resistance, hypertension, and high cholesterol, significantly raises the risk.
- Polycystic Ovary Syndrome (PCOS): This condition is associated with insulin resistance and obesity, increasing the risk of NAFLD.
- Sleep Apnea: Individuals with obstructive sleep apnea may experience worsened liver function and an increased risk of fatty liver.
- Hypothyroidism: An underactive thyroid can contribute to fat buildup in the liver.
Complications of NAFLD
If left untreated, NAFLD can lead to serious health complications, including:
- Liver Fibrosis: Chronic inflammation and liver cell damage can cause scar tissue to form in the liver. Over time, this can lead to fibrosis, which impairs liver function.
- Cirrhosis: As fibrosis progresses, it can lead to cirrhosis, a late stage of liver scarring. Cirrhosis can cause liver failure and increase the risk of liver cancer.
- Liver Cancer: In some cases, NAFLD can progress to hepatocellular carcinoma (HCC), a type of liver cancer.
- Cardiovascular Disease: NAFLD is often associated with an increased risk of heart disease and stroke due to its links with metabolic syndrome.
- End-Stage Liver Disease: Advanced cirrhosis can result in liver failure, requiring a liver transplant for survival.
Diagnosis of NAFLD
NAFLD is often discovered during routine medical exams when abnormal liver enzyme levels are detected. Several methods are used to confirm the diagnosis, including:
- Blood Tests: Liver function tests measure liver enzymes and can indicate inflammation or damage. Additional tests can rule out other causes of liver disease.
- Imaging: Ultrasound, MRI, or CT scans can reveal fat accumulation in the liver.
- Liver Biopsy: In more severe cases, a liver biopsy may be performed to assess the extent of liver damage and inflammation.
Treatment for NAFLD
Currently, no specific medications are approved to treat NAFLD. The treatment primarily focuses on lifestyle modifications and addressing underlying risk factors:
- Weight Loss: Gradual weight loss (5-10% of body weight) can significantly reduce fat in the liver and improve liver function.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins( a protein low in fat and calories but high in protein) can help reduce liver fat. Avoiding sugary, high-fat, and processed foods is essential.
- Exercise: Regular physical activity (at least 150 minutes per week) improves insulin sensitivity, reduces liver fat, and promotes overall health.
- Control of Diabetes and Cholesterol: Managing blood sugar levels, cholesterol, and triglycerides is critical in preventing the progression of NAFLD.
- Medications: Although no drugs are specifically approved for NAFLD, medications like pioglitazone, vitamin E, or statins may be prescribed in some cases to manage diabetes or high cholesterol.
- Liver Transplant: In cases of end-stage liver disease or liver failure, a transplant may be the only option.
Prevention of NAFLD
While NAFLD is a growing health concern, it is largely preventable through lifestyle changes and risk factor management. Here are key preventive measures:
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight through balanced nutrition and regular exercise is the most effective way to prevent NAFLD.
- Eat a Balanced Diet: Focus on a diet rich in fiber, lean proteins, fruits, and vegetables. Limit sugar, refined carbs, and saturated fats.
- Exercise Regularly: Physical activity helps manage weight, improve insulin sensitivity, and reduce liver fat.
- Manage Medical Conditions: Proper management of conditions like diabetes, high cholesterol, and hypertension is crucial in preventing fatty liver disease.
- Avoid Toxins: Limit exposure to environmental toxins and avoid unnecessary use of medications that can stress the liver.
- Avoid Alcohol: Although NAFLD is not caused by alcohol, but drinking alcohol can make it more worse.
Conclusion
Non-alcoholic fatty liver disease is a widespread yet often silent condition that can lead to serious liver-related complications if left unchecked.
It is intricately linked to lifestyle factors, including diet, physical activity, and metabolic health.
By adopting preventive strategies, such as maintaining a healthy weight and managing underlying medical conditions, individuals can significantly reduce their risk of developing NAFLD.
Early diagnosis and proactive management are key to preventing the progression of this disease and safeguarding liver health.
FAQs
1. What causes non-alcoholic fatty liver disease (NAFLD)?
NAFLD is primarily caused by fat accumulation in the liver, often due to insulin resistance, obesity, type 2 diabetes, and high cholesterol.
2. Can NAFLD be reversed?
Yes, in its early stages (simple steatosis), NAFLD can be reversed with lifestyle changes, including weight loss, a healthy diet, and regular exercise.
3. What are the symptoms of non-alcoholic fatty liver disease?
Many people with NAFLD have no symptoms. However, some may experience fatigue, abdominal discomfort, or unexplained weight loss. In more severe cases, symptoms can include jaundice and swelling in the abdomen.
4. What is the difference between NAFLD and NASH?
NAFLD includes simple fatty liver (steatosis) and non-alcoholic steatohepatitis (NASH). NASH is a more severe form that involves liver inflammation and damage.
5. Is non-alcoholic fatty liver disease common in children?
Yes, the incidence of NAFLD is increasing in children, especially those with obesity and insulin resistance.
6. How is NAFLD diagnosed?
NAFLD is often diagnosed through blood tests showing elevated liver enzymes, imaging tests (such as ultrasound), and in some cases, a liver biopsy.
7. Can NAFLD lead to liver cancer?
Yes, if NAFLD progresses to NASH and cirrhosis, it can increase the risk of liver cancer (hepatocellular carcinoma).
8. Are there any dietary recommendations for people with NAFLD?
A balanced diet rich in fruits, vegetables, whole grains, and proteins is recommended. Reducing sugar and saturated fats is also important.
9. Who is at risk for developing NAFLD?
People who are obese, have type 2 diabetes or have high cholesterol or triglycerides are at higher risk. Additionally, those with metabolic syndrome and certain genetic factors may also be at risk.