Overview
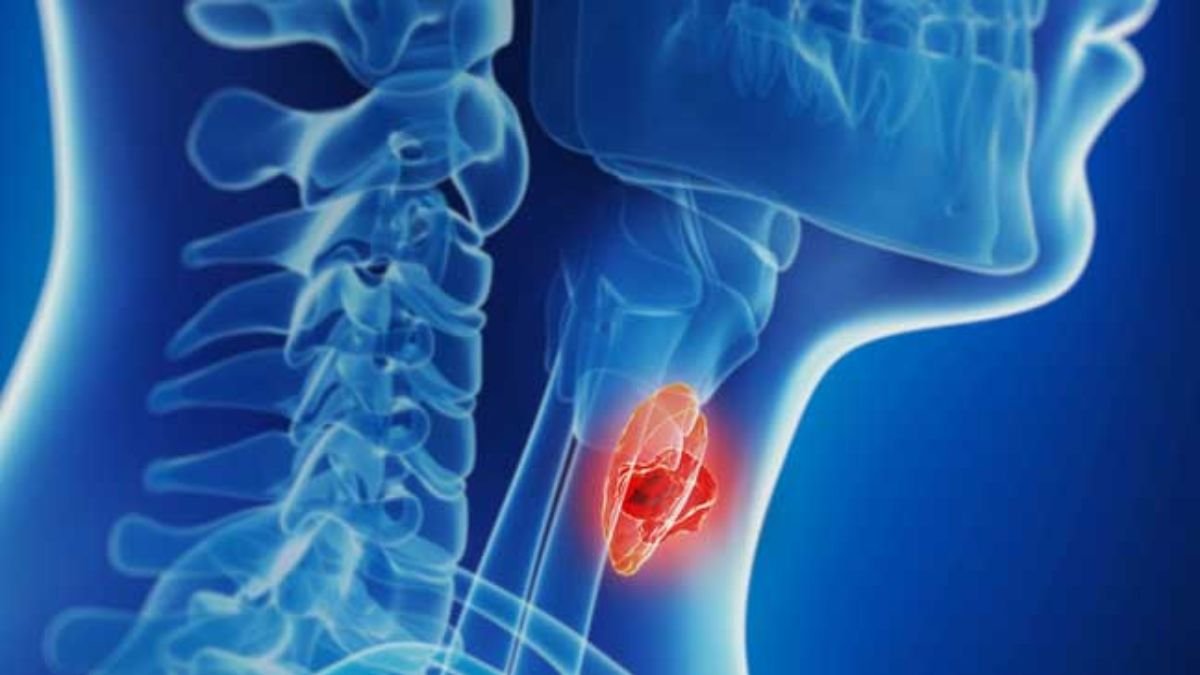
Thyroid nodules are abnormal growths or lumps that develop within the thyroid gland, located at the base of the neck.
These nodules can be solid, fluid-filled (cysts), or a combination of both. Thyroid nodules are quite common, and most are benign (non-cancerous).
However, in some cases, they can be indicative of an underlying thyroid disorder or, more rarely, thyroid cancer.
Many individuals with thyroid nodules do not experience noticeable symptoms, but in some cases, nodules may lead to visible swelling, difficulty swallowing, or thyroid dysfunction.
What is a Thyroid Nodule?
A thyroid nodule is a lump or growth that forms within the thyroid gland. These nodules can vary in size, from tiny nodules that are difficult to detect to larger lumps that can cause visible swelling of the neck.
Types of Thyroid Nodules
Thyroid nodules may be single or multiple, and they can be classified into the following types:
1. Benign (Non-cancerous) Nodules: The majority of thyroid nodules fall into this category and are not harmful.
2. Malignant (Cancerous) Nodules: A small percentage of nodules are cancerous, requiring prompt medical intervention.
3. Cystic Nodules: Fluid-filled nodules that may cause discomfort or compressive symptoms.
4. Solid Nodules: These can be benign adenomas or, in rare cases, malignant tumors.
5. Multinodular Goiter: A condition characterized by multiple nodules forming within the thyroid, often leading to gland enlargement.
Symptoms
Many thyroid nodules do not cause symptoms and are discovered incidentally during a routine physical exam or imaging study for another condition. When symptoms do occur, they may include:
1. Visible Lump or Swelling: A noticeable lump in the neck, often more apparent when swallowing or turning the head.
2. Difficulty Swallowing or Breathing: Large nodules may press on the esophagus or windpipe, causing discomfort.
3. Throat Pain or Discomfort: Some nodules can cause a sensation of fullness, tightness, or pain in the neck.
4. Voice Changes: Nodules pressing on the vocal cords may cause hoarseness or changes in voice quality.
5. Hyperthyroid Symptoms (if nodules produce excess hormones):
- Rapid or irregular heartbeat
- Weight loss despite increased appetite
- Nervousness, anxiety, and tremors
- Excessive sweating
6. Hypothyroid Symptoms (if nodules interfere with hormone production):
- Fatigue and sluggishness
- Weight gain
- Cold intolerance
- Dry skin and hair
Causes
The exact cause of thyroid nodules is often unknown, but several factors may contribute to their development:
1. Iodine Deficiency: A lack of iodine in the diet can lead to the formation of thyroid nodules, as iodine is essential for thyroid hormone production.
2. Thyroiditis: Inflammation of the thyroid, such as in Hashimoto’s thyroiditis, can lead to nodular formation and may cause the gland to enlarge.
3. Genetic Factors: A family history of thyroid nodules, thyroid disease, or autoimmune conditions increases the risk.
4. Benign Tumors (Adenomas): Non-cancerous growths can develop within the thyroid gland, sometimes causing nodules.
5. Multinodular Goiter: This condition occurs when multiple nodules form, causing gland enlargement.
6. Thyroid Cancer: In rare cases, a thyroid nodule may be cancerous, requiring careful evaluation.
7. Radiation Exposure: Individuals exposed to radiation, especially during childhood, have a higher risk of developing thyroid nodules.
8. Hormonal Imbalances: Hormonal changes during pregnancy, menopause, or due to certain medications may contribute to nodular growth.
Risk Factors
Certain factors increase the likelihood of developing thyroid nodules:
1. Age and Gender: Thyroid nodules are more common in women and older individuals.
2. Family History: A family history of thyroid nodules or thyroid cancer increases risk.
3. Radiation Exposure: Previous radiation therapy to the neck or head area raises the risk.
4. Iodine Deficiency: Inadequate iodine intake remains a significant risk factor in areas with iodine-deficient diets.
5. Chronic Thyroid Inflammation: Autoimmune conditions such as Hashimoto’s thyroiditis may lead to nodular formation.
Complications
- Compression Symptoms: Large nodules may press on the windpipe or esophagus, causing difficulty breathing or swallowing.
- Hyperthyroidism or Hypothyroidism: Some nodules may alter hormone production, leading to thyroid dysfunction.
- Cancer: A small percentage of nodules are malignant, requiring timely diagnosis and treatment.
Diagnosis
The diagnosis of thyroid nodules typically involves the following steps:
1. Physical Examination: A healthcare provider examines the neck for lumps or swelling and may feel the size and texture of the thyroid gland.
2. Blood Tests: Thyroid function tests measure levels of thyroid-stimulating hormone (TSH) and thyroid hormones (T3, T4) to assess whether the thyroid is underactive, overactive, or functioning normally.
3. Ultrasound: An ultrasound of the thyroid helps determine the size, shape, and composition (solid or cystic) of the nodule(s) and can identify suspicious features.
4. Fine-Needle Aspiration (FNA) Biopsy: A thin needle is used to collect cells from the nodule for examination under a microscope to rule out cancer.
5. Thyroid Scan: In some cases, a radioactive iodine scan can help evaluate thyroid function and distinguish between different types of nodules.
Treatment
Treatment for thyroid nodules depends on their size, type, symptoms, and whether they are benign or malignant:
1. Observation: If a nodule is small, asymptomatic, and non-cancerous, regular monitoring with periodic ultrasound and thyroid function tests may be recommended.
2. Medications:
- Thyroid Hormone Suppression Therapy: In some cases, thyroid hormone medications may be used to reduce the size of nodules by lowering TSH stimulation.
- Antithyroid Drugs: If the nodule is causing hyperthyroidism, medications may be prescribed to reduce hormone production.
3. Radioactive Iodine Therapy: This therapy may shrink nodules associated with hyperthyroidism by destroying overactive thyroid tissue.
4. Surgery (Thyroidectomy): Surgical removal of part or all of the thyroid may be necessary for large nodules, nodules causing symptoms, or nodules suspected of being cancerous.
Prevention
While not all thyroid nodules can be prevented, some measures may reduce the risk:
1. Adequate Iodine Intake: Consuming iodized salt and iodine-rich foods, such as seafood and dairy, supports thyroid health.
2. Avoid Unnecessary Radiation Exposure: Limit radiation exposure, particularly to the head and neck, unless medically necessary.
3. Regular Check-ups: Routine thyroid exams can catch nodules early, especially if you have risk factors such as a family history or past radiation exposure.
4. Balanced Diet: A healthy diet rich in essential nutrients can support overall thyroid health.
Conclusion
Thyroid nodules are common and often benign, but they can sometimes indicate underlying thyroid dysfunction or, more rarely, cancer.
Proper diagnosis through physical exams, imaging, and biopsy is essential to determine the best course of action.
Depending on the characteristics of the nodule, treatment options range from observation to medication or surgery.
By maintaining regular thyroid health checks and a balanced diet, individuals can better manage or prevent thyroid nodules and associated complications.
FAQs
1. Are all thyroid nodules cancerous?
No, the vast majority of thyroid nodules are benign and not cancerous. Only a small percentage may be malignant.
2. How are thyroid nodules detected?
Most nodules are discovered during routine exams or imaging studies. Ultrasound and fine-needle biopsy help evaluate their nature.
3. Can thyroid nodules go away on their own?
Some nodules, especially cystic ones, may shrink or resolve over time. Others may persist and require monitoring.
4. Are thyroid nodules common?
Yes, thyroid nodules are quite common, especially in women and older adults.
5. What causes thyroid nodules?
Common causes include iodine deficiency, autoimmune thyroid disease, genetic factors, and thyroid inflammation.