Overview:
Diabetes is a chronic health condition that occurs when the body is unable to properly regulate blood sugar (glucose) levels.
Glucose is a primary energy source for the body’s cells, but for it to be used efficiently, the hormone insulin is required.
In people with diabetes, either the body does not produce enough insulin or the cells do not respond properly to insulin, leading to elevated blood glucose levels.
Over time, high blood sugar can cause severe damage to various organs, including the heart, kidneys, eyes, and nerves.
With the global prevalence of diabetes on the rise, it is becoming a major health challenge. According to the International Diabetes
Federation, approximately 537 million adults worldwide were living with diabetes in 2021. Understanding the nature of diabetes, its symptoms, causes, and how to manage it can help prevent complications and improve quality of life.
This blog provides an in-depth overview of diabetes, covering everything from its types to effective management strategies.
Table of Contents
What is Diabetes?
Diabetes is a metabolic disorder characterized by high blood sugar levels over a prolonged period.
Types Of Diabetes
There are three main types of diabetes:
1. Type 1 Diabetes: An autoimmune condition in which the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. As a result, the body produces little or no insulin, necessitating lifelong insulin therapy. Type 1 diabetes usually develops in childhood or adolescence but can occur at any age.
2. Type 2 Diabetes: The most common type of diabetes, Type 2 occurs when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin to meet the body’s needs. It is often associated with lifestyle factors such as obesity, sedentary behavior, and poor dietary habits. Type 2 diabetes typically develops in adults but is increasingly seen in younger individuals.
3. Gestational Diabetes: This type of diabetes occurs during pregnancy and usually resolves after childbirth. However, women who have had gestational diabetes are at higher risk of developing Type 2 diabetes later in life.
There is also a condition known as Prediabetes, in which blood sugar levels are higher than normal but not high enough to be classified as diabetes. Prediabetes increases the risk of developing Type 2 diabetes and cardiovascular disease.
Symptoms of Diabetes
The symptoms of diabetes can vary depending on the type and severity of the condition. Some individuals may not experience any symptoms, especially in the early stages of Type 2 diabetes. However, common symptoms include:
- Frequent Urination (Polyuria): Elevated blood glucose levels cause the kidneys to work harder to remove excess sugar, resulting in frequent urination.
- Excessive Thirst (Polydipsia): As the body loses more fluids through frequent urination, dehydration can occur, leading to increased thirst.
- Increased Hunger (Polyphagia): Despite eating more, individuals with diabetes may experience constant hunger because the body’s cells are not able to utilize glucose effectively for energy.
- Unexplained Weight Loss: Rapid weight loss, especially in Type 1 diabetes, occurs when the body breaks down muscle and fat for energy in the absence of sufficient insulin.
- Fatigue and Weakness: Lack of energy due to the body’s inability to use glucose properly can result in persistent tiredness.
- Blurred Vision: High blood sugar levels can cause swelling in the lens of the eye, leading to blurred vision.
- Slow-Healing Wounds and Infections: Poor circulation and high blood sugar can impair the body’s ability to heal wounds and fight infections.
- Tingling or Numbness in Hands and Feet: Over time, high blood sugar can damage nerves, causing tingling, numbness, or pain (a condition known as diabetic neuropathy).
It is essential to recognize these symptoms and seek medical advice for early diagnosis and intervention.
Causes of Diabetes
The causes of diabetes vary depending on its type:
1. Type 1 Diabetes:
The exact cause of Type 1 diabetes is not fully understood. However, it is believed to be an autoimmune condition in which the immune system attacks insulin-producing beta cells in the pancreas. Genetic predisposition and environmental factors, such as viral infections, may play a role in triggering the onset of Type 1 diabetes.
2. Type 2 Diabetes:
Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin to maintain normal blood sugar levels. Factors that contribute to insulin resistance include obesity, a sedentary lifestyle, poor diet, and genetic predisposition.
3. Gestational Diabetes:
Gestational diabetes occurs when the body cannot produce enough insulin to meet the increased needs during pregnancy. Hormonal changes and weight gain are believed to contribute to this condition.
4. Prediabetes:
The same factors that increase the risk of developing Type 2 diabetes—such as obesity, physical inactivity, and family history—can lead to prediabetes.
Risk Factors of Diabetes
Several risk factors can increase the likelihood of developing diabetes. These risk factors can be categorized into modifiable and non-modifiable factors:
Modifiable Risk Factors:
- Obesity: Excess body weight, especially around the abdomen, is a major risk factor for Type 2 diabetes.
- Physical Inactivity: A sedentary lifestyle contributes to obesity and increases insulin resistance.
- Poor Diet: Diets high in processed foods, sugary beverages, and unhealthy fats can raise the risk of diabetes.
- Smoking: Smoking is associated with a higher risk of diabetes and complications, such as heart disease and kidney damage.
- Excessive Alcohol Consumption: Heavy alcohol use can increase the risk of Type 2 diabetes.
Non-Modifiable Risk Factors:
- Family History: Having a close relative with diabetes increases the risk of developing the condition.
- Age: The risk of Type 2 diabetes increases with age, especially after 45.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, Native Americans, and Asian Americans, have a higher risk of developing diabetes.
- History of Gestational Diabetes: Women who have had gestational diabetes are more likely to develop Type 2 diabetes later in life.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS are at increased risk of diabetes due to insulin resistance.
Treatment for Diabetes
The treatment of diabetes aims to manage blood sugar levels and prevent complications. The treatment plan varies depending on the type of diabetes:
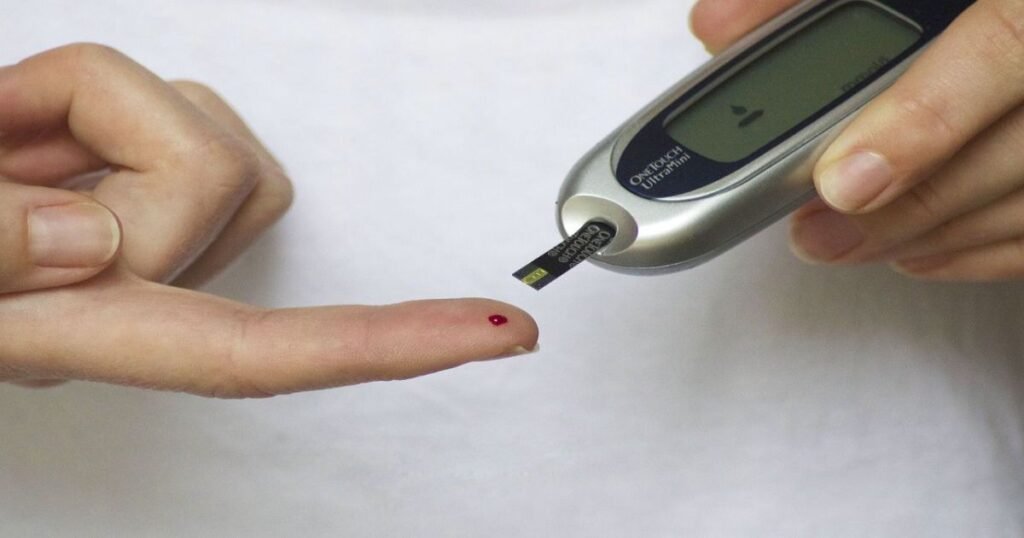
- Type 1 Diabetes: Since the body cannot produce insulin, individuals with Type 1 diabetes require lifelong insulin therapy. Insulin can be administered through injections or an insulin pump. Regular blood sugar monitoring, a balanced diet, and physical activity are also crucial for managing Type 1 diabetes.
- Type 2 Diabetes: Treatment options for Type 2 diabetes include lifestyle modifications (diet and exercise), oral medications, and insulin therapy if necessary.
- Gestational Diabetes: Treatment typically involves dietary changes, regular exercise, and blood sugar monitoring. In some cases, insulin therapy may be necessary to control blood sugar levels during pregnancy.
- Prediabetes: Lifestyle interventions, including weight loss, a healthy diet, and increased physical activity, can prevent the progression of prediabetes to Type 2 diabetes.
Prevention of Diabetes
Preventing diabetes involves adopting a healthy lifestyle and managing risk factors. Here are some strategies to reduce the risk of diabetes:
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight through a balanced diet and regular physical activity can significantly reduce the risk of Type 2 diabetes.
- Follow a Healthy Diet: Choose a diet rich in whole grains, proteins, fruits, and vegetables, and low in saturated fats, trans fats, and added sugars.
- Engage in Regular Physical Activity: Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking or cycling, each day.
- Quit Smoking: If you smoke, quitting can improve overall health and reduce the risk of diabetes and other chronic conditions.
- Avoid Alcohol Consumption: Drinking alcohol can increase the risk of diabetes and other health problems.
- Manage Stress: Chronic stress can lead to unhealthy behaviors and insulin resistance. Practice stress-reduction techniques such as meditation, deep breathing, or yoga.
- Get Regular Health Checkups: Regular screenings for blood sugar levels can help identify prediabetes or diabetes early, enabling timely intervention.
Key Takeaways
Diabetes is a serious and lifelong condition that requires careful management.
However, with the right combination of diet, exercise, medications, and regular monitoring, individuals with diabetes can lead healthy and active lives.
Recognizing the symptoms and understanding the risk factors are the first steps toward managing diabetes effectively.
By adopting a healthy lifestyle and following medical advice, the risk of complications can be significantly reduced.
Through awareness and proactive measures, the global burden of diabetes can be mitigated, leading to better outcomes for individuals and communities alike.
FAQs
1. What is the difference between Type 1 and Type 2 diabetes?
Type 1 diabetes is an autoimmune condition in which the body attacks insulin-producing cells, leading to little or no insulin production. Type 2 diabetes is primarily a result of insulin resistance and often occurs due to lifestyle factors.
2. Can diabetes be cured?
There is currently no cure for diabetes, but it can be effectively managed. With proper treatment, lifestyle changes, and ongoing medical care, individuals with diabetes can keep their blood sugar levels in check and prevent complications.
3. Is diabetes reversible?
While Type 1 diabetes is not reversible, some people with Type 2 diabetes can achieve remission through significant lifestyle changes such as weight loss, a healthy diet, and increased physical activity. Remission means that blood sugar levels remain within a healthy range without the need for diabetes medications, but it does not mean that the condition is completely cured.
4. What foods should I avoid if I have diabetes?
People with diabetes should limit or avoid foods high in refined sugars, unhealthy fats (e.g., trans fats and saturated fats), and simple carbohydrates. This includes sugary drinks, processed snacks, fried foods, white bread, and pastries. Instead, focus on consuming whole grains, lean proteins, healthy fats, and a variety of vegetables.
5. How does diabetes affect the body?
Diabetes can have widespread effects on the body if not managed properly. High blood sugar levels can damage blood vessels and nerves, leading to complications such as heart disease, kidney disease, nerve damage (neuropathy), eye problems (retinopathy), and an increased risk of infections and slow wound healing.
6. Can exercise help manage diabetes?
Yes, regular exercise can help manage diabetes by improving insulin sensitivity, lowering blood sugar levels, promoting weight loss, and enhancing overall health. It is recommended to engage in at least 30 minutes of moderate-intensity exercise each day, along with strength training activities.
7. What are the long-term complications of diabetes?
Long-term complications of diabetes include cardiovascular disease (heart attack and stroke), kidney damage (diabetic nephropathy), nerve damage (diabetic neuropathy), vision problems (diabetic retinopathy), and foot complications, which can lead to infections and, in severe cases, amputation.
8. Can stress cause diabetes?
While stress itself does not directly cause diabetes, it can contribute to behaviors and physiological changes that increase the risk. Chronic stress can lead to unhealthy habits such as overeating, physical inactivity, and poor sleep, all of which contribute to weight gain and insulin resistance.
9. How can I prevent diabetes if I am at high risk?
If you are at high risk of developing diabetes (e.g., due to family history, obesity, or prediabetes), adopting a healthy lifestyle can significantly lower your risk. Focus on maintaining a healthy weight, eating a balanced diet, staying physically active, and avoiding smoking and excessive alcohol consumption. Regular screenings for blood sugar levels can also help detect early signs of diabetes.
10. What is diabetic ketoacidosis (DKA)?
Diabetic ketoacidosis (DKA) is a serious and potentially life-threatening complication of diabetes, primarily Type 1 diabetes. It occurs when the body produces high levels of ketones (acids) due to the lack of insulin. Symptoms include extreme thirst, frequent urination, nausea, vomiting, abdominal pain, and confusion. DKA requires immediate medical attention.
11. Is diabetes genetic?
Yes, genetics play a role in the development of both Type 1 and Type 2 diabetes. Having a family history of diabetes increases the risk, but environmental and lifestyle factors also contribute to the onset of the condition.
12. Can people with diabetes eat fruits?
Yes, people with diabetes can eat fruits in moderation as part of a balanced diet. Choose fruits with a low glycemic index (GI) like berries, apples, and citrus fruits, and avoid consuming them in large quantities. It’s also a good idea to pair fruits with a source of protein or healthy fat to minimize spikes in blood sugar levels.
13. What are the early signs of diabetes in children?
Early signs of diabetes in children include increased thirst and urination, unexplained weight loss, fatigue, irritability, and sudden changes in vision. If these symptoms are noticed, it is crucial to seek medical advice for an early diagnosis and management plan.
14. How often should people with diabetes check their blood sugar levels?
The frequency of blood sugar monitoring depends on the type of diabetes and the treatment plan. People with Type 1 diabetes or those taking insulin should check their blood sugar levels multiple times a day. Individuals with Type 2 diabetes may not need to check as frequently, depending on their treatment plan and blood sugar control. It’s best to follow the recommendations of your healthcare provider.
15. What is the role of medication in managing diabetes?
Medications play a crucial role in managing diabetes by controlling blood sugar levels. For Type 1 diabetes, insulin is required for life. For Type 2 diabetes, various oral medications (such as metformin) and injectable drugs can help regulate blood sugar. In some cases, insulin therapy may also be necessary. Your healthcare provider will determine the best medication plan based on your condition.

