Overview
Hyperglycemia, or high blood sugar, is a condition where blood glucose levels rise above the normal range. While it’s common among people with diabetes, hyperglycemia can occasionally affect non-diabetic individuals under certain conditions.
Blood glucose is the primary source of energy for the body, especially the brain, and is regulated by hormones like insulin.
When blood sugar remains elevated over an extended period, it can lead to various complications, including damage to the eyes, kidneys, and nerves.
Recognizing and managing hyperglycemia is critical to maintaining optimal health, especially for those with diabetes.
Table of Contents
What is Hyperglycemia?

Hyperglycemia is defined as blood glucose levels above the normal range, typically higher than 130 mg/dL (7.2 mmol/L) when fasting and over 180 mg/dL (10 mmol/L) two hours after meals.
Occasional spikes in blood sugar may not cause immediate harm, but persistent hyperglycemia can lead to significant health risks over time, including cardiovascular disease and nerve damage.
Hyperglycemia is most often associated with diabetes, where the body’s ability to regulate blood glucose is compromised.
It can occur in both Type 1 and Type 2 diabetes and may also affect people under physical or emotional stress, those taking certain medications, or individuals with certain metabolic conditions.
Symptoms of Hyperglycemia
Hyperglycemia symptoms can vary in intensity depending on how high blood glucose levels are and how long they have been elevated. Symptoms are generally divided into early and advanced stages.
Early Symptoms
In the early stages, hyperglycemia may present mild symptoms, which, if recognized early, can help prevent complications:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Blurred vision
- Fatigue or general tiredness
- Headaches
- Dry mouth
Advanced Symptoms
If hyperglycemia is left untreated, it can worsen and lead to more severe symptoms, particularly in cases of extremely high blood sugar levels:
- Nausea and vomiting
- Shortness of breath
- Abdominal pain
- Confusion or difficulty concentrating
- Fruity-smelling breath (a sign of diabetic ketoacidosis)
In severe cases, hyperglycemia can result in a dangerous condition known as diabetic ketoacidosis (DKA) in Type 1 diabetes or hyperosmolar hyperglycemic state (HHS) in Type 2 diabetes, both of which require immediate medical attention.
Causes of Hyperglycemia
Hyperglycemia occurs when the body has too little insulin or cannot use insulin effectively, leading to elevated blood glucose levels. Several factors can contribute to hyperglycemia:
1. Insufficient Insulin Production
- Type 1 Diabetes: The body’s immune system attacks insulin-producing cells in the pancreas, leading to an inability to produce insulin.
- Type 2 Diabetes: The body becomes resistant to insulin, or the pancreas does not produce enough insulin to meet the body’s needs.
2. Poor Medication Adherence: Missing insulin doses or other diabetes medications can cause blood glucose levels to rise. Inconsistent medication adherence is a common cause of hyperglycemia in people with diabetes.
3. Dietary Choices: Consuming foods high in sugar or carbohydrates without adequate insulin can cause blood glucose levels to spike. In people with diabetes, improper meal planning can significantly affect blood sugar levels.
4. Stress and Illness: Physical stress from illness, surgery, or infection, as well as emotional stress, can trigger the release of stress hormones, such as cortisol, which increases blood glucose.
5. Lack of Physical Activity: Physical inactivity can worsen insulin resistance, especially in individuals with Type 2 diabetes, making it harder for cells to absorb glucose from the bloodstream.
6. Certain Medications: Medications such as steroids, diuretics, and antipsychotic drugs can interfere with blood sugar regulation, causing blood glucose levels to rise.
Risk Factors for Hyperglycemia
Hyperglycemia is most common in people with diabetes, but other factors can also increase the risk:
- Diabetes: Both Type 1 and Type 2 diabetes patients are at higher risk due to impaired insulin function.
- Sedentary Lifestyle: Physical inactivity increases insulin resistance.
- Poor Dietary Choices: Consuming high-sugar, high-carb foods without managing insulin or diabetes medication can lead to elevated blood sugar.
- Obesity: Excess body weight, particularly around the abdomen, is linked to insulin resistance, increasing the risk of hyperglycemia.
- High-Stress Levels: Both physical and emotional stress can raise blood sugar.
- Chronic Illness or Infection: Conditions that affect insulin regulation, like Cushing’s syndrome, can contribute to hyperglycemia.
Complications of Hyperglycemia
If untreated, hyperglycemia can lead to serious complications. Key risks include:
- Diabetic Ketoacidosis (DKA): Common in Type 1 diabetes, DKA arises from fat breakdown-producing ketones, causing nausea, abdominal pain, and a fruity breath. It’s a medical emergency.
- Hyperosmolar Hyperglycemic State (HHS): Found in Type 2 diabetes, HHS involves extreme dehydration and high fever, requiring immediate hospitalization.
- Cardiovascular Disease: High blood sugar harms blood vessels, raising risks of heart disease and stroke.
- Neuropathy: Damaged nerves cause tingling and numbness, especially in extremities, leading to infection risks.
- Nephropathy: Kidney damage can result in failure, needing dialysis or transplant.
- Retinopathy: High glucose damages retinal blood vessels, risking vision loss.
- Skin Issues: High sugar raises susceptibility to infections and poor wound healing.
- Cognitive Decline: Prolonged hyperglycemia may affect memory and judgment.
Managing blood sugar, regular check-ups, and proactive care are essential to prevent these complications and protect long-term health.
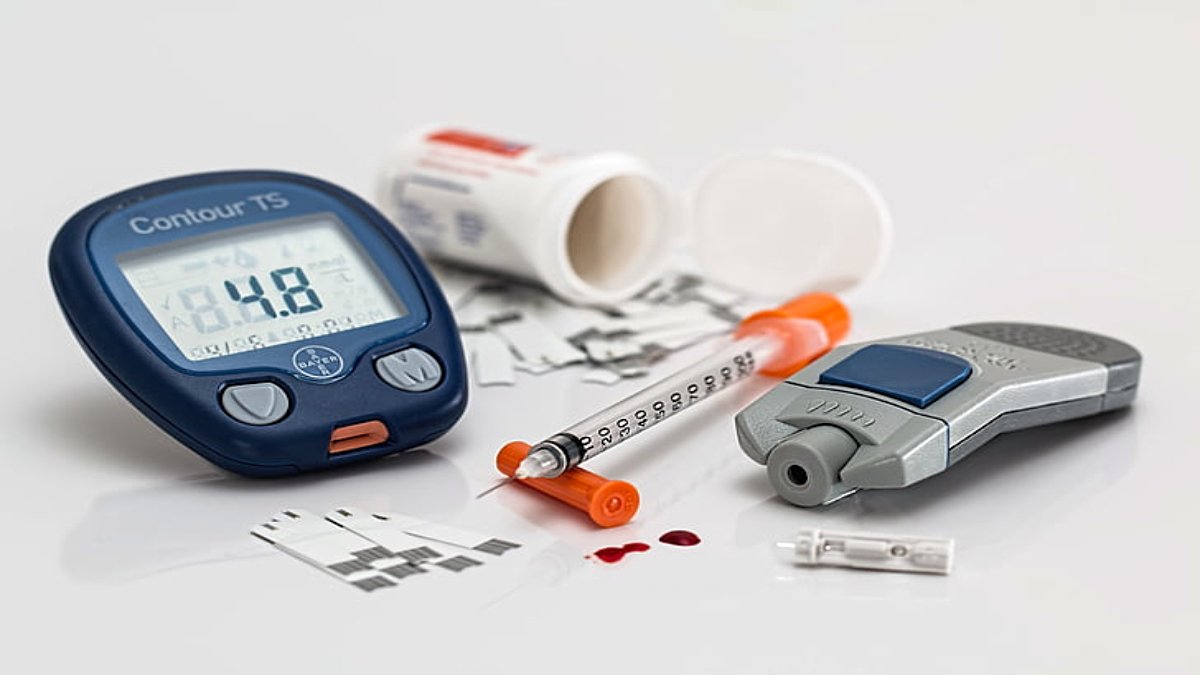
Diagnosis of Hyperglycemia
Healthcare providers use several methods to diagnose hyperglycemia and evaluate blood glucose levels over time:
- Fasting Blood Glucose Test: Measures blood glucose after an overnight fast. Levels above 130 mg/dL indicate hyperglycemia.
- Oral Glucose Tolerance Test (OGTT): Measures blood glucose before and after drinking a sugary solution. Elevated levels post-consumption indicate glucose intolerance.
- A1C Test: Also known as hemoglobin A1c, this test measures average blood glucose over the past 2-3 months. An A1C above 6.5% suggests hyperglycemia in diabetic patients.
- Random Blood Glucose Test: Measures blood glucose at any given time; levels over 200 mg/dL often indicate hyperglycemia, especially in symptomatic individuals.
Treatment of Hyperglycemia
Treatment for hyperglycemia focuses on reducing blood glucose levels to prevent complications. Approaches vary depending on the severity of hyperglycemia and whether the patient has diabetes.
1. Insulin Administration: People with Type 1 diabetes or severe Type 2 diabetes may require insulin injections to lower blood glucose levels rapidly. Dosages may vary based on blood sugar readings.
2. Oral Medications: In cases of Type 2 diabetes, medications such as metformin, sulfonylureas, or DPP-4 inhibitors help improve blood sugar control by increasing insulin sensitivity or reducing glucose production.
3. Dietary Adjustments: Limiting carbohydrate intake and choosing foods with a low glycemic index (GI) can help control blood sugar levels. Monitoring portion sizes and carb intake can also help prevent blood sugar spikes.
4. Physical Activity: Engaging in regular exercise can help lower blood sugar levels by improving insulin sensitivity. Light to moderate activity is usually safe for people with hyperglycemia, but it’s best to check blood sugar before and after exercise.
5. Stress Management: Practicing relaxation techniques, such as mindfulness, yoga, and deep breathing exercises, can help lower stress-induced hyperglycemia.
Preventing Hyperglycemia
Proactive strategies are essential for preventing hyperglycemia, particularly for people with diabetes or those at risk. Here are several preventive measures:
- Monitor Blood Sugar Levels Regularly: Routine blood glucose monitoring can alert individuals to changes, allowing for prompt adjustments in diet or medication.
- Follow a Balanced Diet: Prioritize a diet rich in whole grains, lean proteins, vegetables, and low-GI carbohydrates. Avoid sugary snacks and beverages, which can cause blood sugar spikes.
- Exercise Regularly: Incorporating physical activity, like walking, swimming, or cycling, into a daily routine can significantly improve blood sugar control.
- Take Medications as Prescribed: Adhering to prescribed medications for diabetes or other conditions can prevent hyperglycemia.
- Manage Stress: Engage in activities that reduce stress and promote relaxation, as high stress levels can contribute to elevated blood sugar.
- Stay Hydrated: Drinking enough water can help the body eliminate excess glucose through urine and maintain proper hydration levels.
Conclusion
Hyperglycemia, though common among people with diabetes, can have significant health impacts if not properly managed.
Recognizing the symptoms, understanding the underlying causes, and implementing effective prevention and treatment strategies are essential for maintaining healthy blood sugar levels.
For those with diabetes, monitoring blood glucose, maintaining a balanced diet, and taking medications as prescribed are foundational steps in controlling hyperglycemia.
By managing blood sugar proactively, individuals can prevent complications and lead a healthier, more balanced life.
Frequently Asked Questions (FAQs)
1. Can hyperglycemia occur in non-diabetics?
Yes, hyperglycemia can occur in non-diabetics, particularly in people who are stressed, ill, inactive, or taking medications that affect blood sugar levels.
2. How is hyperglycemia different from hypoglycemia?
Hyperglycemia is high blood sugar, while hypoglycemia refers to low blood sugar. Both can have serious health effects and require different treatments and preventive strategies.
3. Can hyperglycemia cause permanent damage?
Yes, chronic hyperglycemia can lead to complications like nerve damage, kidney disease, and vision problems, particularly if left unmanaged.
4. What should I do if my blood sugar is consistently high?
Consult a healthcare provider to evaluate your medication, diet, and lifestyle. Adjustments to your treatment plan may be necessary to lower blood sugar levels safely.
5. Can exercise reduce hyperglycemia?
Yes, regular physical activity can help improve insulin sensitivity, which aids in reducing high blood sugar levels.