Overview
High-density lipoprotein (HDL), often termed the “good” cholesterol, plays a crucial role in cardiovascular health.
Unlike its counterpart, low-density lipoprotein (LDL), which can lead to plaque buildup in the arteries, HDL helps remove cholesterol from the bloodstream and transport it to the liver for excretion.
Maintaining optimal HDL levels is essential for reducing the risk of heart disease, stroke, and other cardiovascular complications.
This blog provides a comprehensive understanding of high-density lipoprotein (HDL), its functions, the factors influencing its levels, and how to optimize it for better heart health.
Table of Contents
What is High-Density Lipoprotein (HDL)?
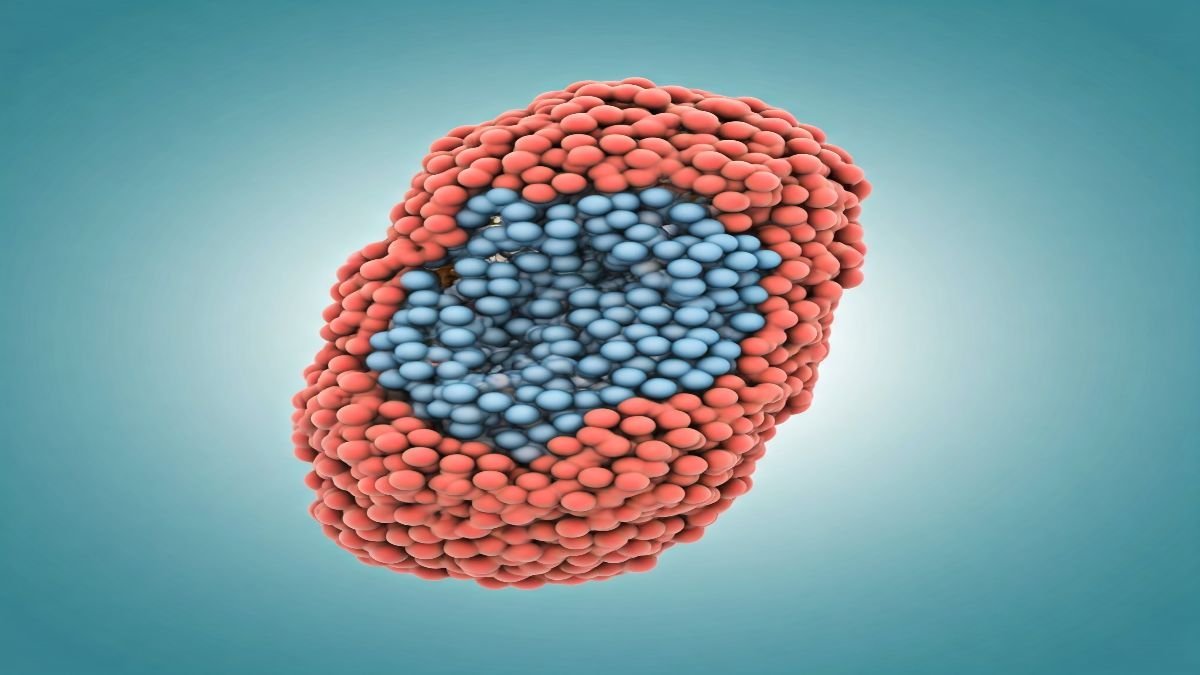
HDL is one of the five major types of lipoproteins responsible for transporting cholesterol and other lipids in the blood.
HDL particles are smaller and denser than LDL, making them highly efficient in scavenging excess cholesterol.
By removing cholesterol from the arteries, HDL reduces the risk of atherosclerosis and other cardiovascular diseases.
Functions of HDL
- Reverse Cholesterol Transport: HDL collects excess cholesterol from tissues and arterial walls and delivers it to the liver for metabolism or excretion through bile.
- Antioxidant Properties: HDL protects LDL from oxidative damage, reducing the formation of harmful oxidized LDL, a key contributor to plaque formation.
- Anti-Inflammatory Effects: HDL helps reduce inflammation in blood vessels, maintaining their flexibility and preventing damage.
- Endothelial Protection: HDL supports the health of the endothelium (the inner lining of blood vessels), ensuring proper blood flow.
Optimal HDL Levels
According to health guidelines, the desirable HDL levels are:
- Men: 40 mg/dL or higher
- Women: 50 mg/dL or higher
- Optimal: 60 mg/dL or higher (associated with a lower risk of heart disease)
Levels below the recommended thresholds may increase the risk of cardiovascular complications.
Symptoms of Low HDL Levels
Low HDL cholesterol itself does not cause specific symptoms. However, its deficiency may lead to cardiovascular complications over time:
- Increased Risk of Atherosclerosis: Excess cholesterol accumulates in arteries due to inadequate removal by HDL.
- Chest Pain (Angina): Resulting from reduced blood flow to the heart due to arterial narrowing.
- Stroke or Heart Attack: Plaque buildup and rupture in arteries can cause life-threatening events.
- Fatigue and Weakness: Caused by reduced oxygen supply to muscles and tissues.
Causes of Low HDL Levels
Several factors can contribute to reduced HDL cholesterol, including:
- Poor Diet: Diets high in refined carbohydrates, trans fats, and added sugars lower HDL levels.
- Lack of Physical Activity: Sedentary lifestyles decrease HDL production and reduce its efficiency in cholesterol removal.
- Obesity: Excess body fat negatively impacts cholesterol metabolism, leading to lower HDL levels.
- Smoking: Smoking damages HDL particles, reducing their cholesterol-removing capacity.
- Medical Conditions: Conditions like diabetes, metabolic syndrome, and chronic inflammation can lower HDL.
- Genetics: Genetic factors influence the amount and functionality of HDL in the body.
- Alcohol Consumption: Excessive drinking can reduce HDL.
Complications of Low HDL Levels
When untreated, low HDL levels can result in severe health conditions:
- Heart Attack: Low HDL fails to prevent cholesterol buildup in coronary arteries.
- Stroke: Reduced cholesterol clearance increases the risk of cerebrovascular blockages.
- Chronic Kidney Disease: Poor vascular health affects renal arteries, impairing kidney function.
- Peripheral Artery Disease: Blood flow to limbs is compromised, leading to pain and potential tissue damage.
Diagnosis of Low HDL Levels
HDL levels are assessed through a lipid panel, a blood test measuring:
- Total Cholesterol: Overall cholesterol in the blood, including LDL and HDL.
- LDL Cholesterol: The “bad” cholesterol contributes to plaque buildup.
- Triglycerides: High levels of this fat can indirectly lower HDL cholesterol.
- HDL Cholesterol: Direct measurement of HDL concentration in the blood.
Health Risks of Low HDL Levels
Reduced HDL levels are associated with:
- Atherosclerosis: Narrowing and hardening of arteries due to cholesterol buildup.
- Coronary Artery Disease (CAD): Low HDL increases the likelihood of plaque formation in coronary arteries.
- Stroke: Cholesterol deposits in brain arteries can lead to ischemic stroke.
- Peripheral Artery Disease (PAD): Poor cholesterol clearance leads to restricted blood flow in the limbs.
- Type 2 Diabetes Risk: Low HDL is often linked to insulin resistance and metabolic syndrome.
Treatment Options for Low HDL Cholesterol
Improving HDL levels involves a combination of lifestyle changes and medical interventions:
Lifestyle Modifications
- Healthy Diet: Incorporate foods rich in healthy fats, such as avocados, nuts, and seeds. Omega-3 fatty acids, found in plant oils and walnuts, are particularly beneficial for raising HDL.
- Exercise Regularly: Aerobic activities like walking, jogging, or cycling for 30 minutes daily can significantly boost HDL.
- Weight Management: Losing excess weight improves HDL cholesterol and reduces cardiovascular risks.
- Quit Smoking: Eliminating tobacco improves HDL function and overall heart health.
- Limit Refined Sugars and Carbohydrates: Focus on whole grains, fruits, and vegetables to improve cholesterol balance.
- Avoid Alcohol Intake: Avoid consumption of alcohol as there is no amount of alcohol that is good for your health.
Medications
- Niacin (Vitamin B3): Proven to raise HDL levels and improve cholesterol ratios.
- Statins: Although primarily used to lower LDL, statins can have a modest effect on raising HDL.
- Fibrates: Effective for increasing HDL and reducing triglycerides.
- Cholesterol Absorption Inhibitors: Medications like ezetimibe help manage cholesterol balance, indirectly improving HDL.
Preventing Low HDL Cholesterol
Preventative strategies focus on maintaining a healthy lifestyle:
- Adopt a Balanced Diet: Prioritize heart-healthy foods like olive oil, leafy greens, and legumes.
- Stay Physically Active: Engage in both aerobic and strength-training exercises.
- Regular Health Check-Ups: Early detection of imbalances in cholesterol can prevent long-term complications.
- Control Blood Sugar Levels: Managing diabetes and avoiding sugary foods help maintain HDL levels.
- Avoid Smoking: Tobacco cessation preserves HDL cholesterol and overall vascular health.
Conclusion
High-density lipoprotein (HDL) is essential for cardiovascular health, earning its reputation as the “good cholesterol.”
By removing excess cholesterol from the bloodstream, HDL helps prevent heart disease, stroke, and other complications.
Maintaining optimal HDL levels through healthy lifestyle choices, regular exercise, and, if necessary, medications, is vital for long-term wellness.
Regular monitoring and proactive measures can significantly reduce the risks associated with low HDL levels.
FAQs
1. What are normal HDL levels?
For men, 40 mg/dL or higher; for women, 50 mg/dL or higher. Levels above 60 mg/dL are considered protective against heart disease.
2. Can you raise HDL naturally?
Yes, regular exercise, a healthy diet, quitting smoking, and weight loss can naturally boost HDL levels.
3. Does alcohol affect HDL?
Excess alcohol consumption can reduce HDL levels.
4. Are high HDL levels always good?
Extremely high HDL levels (above 100 mg/dL) may indicate genetic disorders or other health issues and should be evaluated by a doctor.
5. How often should I check my HDL levels?
Adults should check their cholesterol levels every 4-6 years or more frequently if they have risk factors for heart disease.