Overview
Peripheral Artery Disease (PAD) is a common circulatory condition that affects the arteries outside the heart, primarily in the legs.
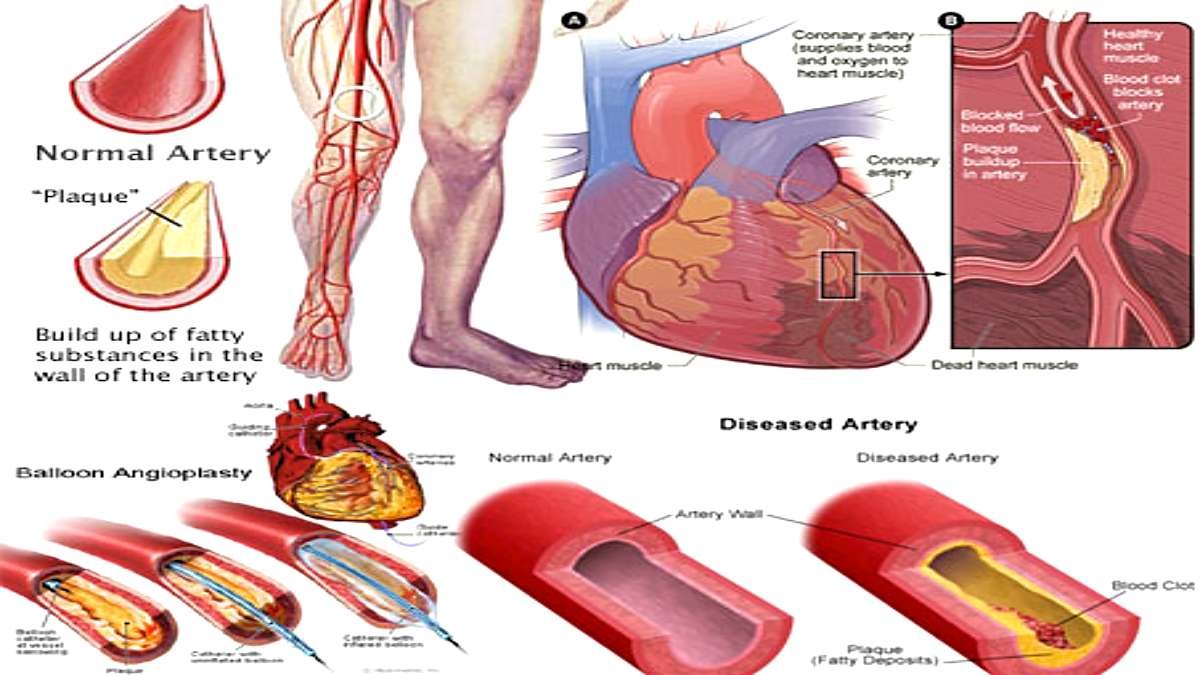
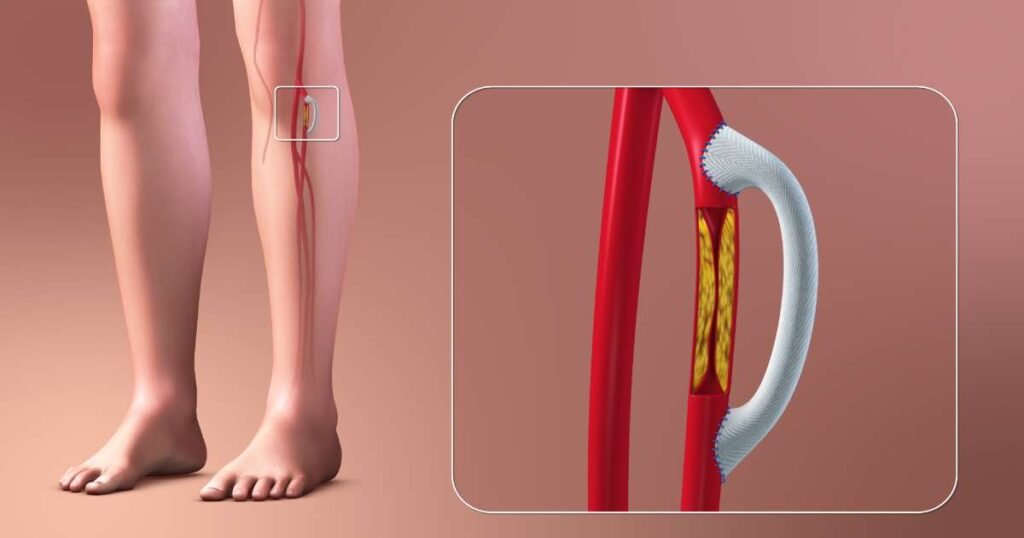
PAD occurs when these arteries become narrowed or blocked due to the buildup of fatty deposits (atherosclerosis), reducing blood flow to the limbs.
This can lead to pain, numbness, and other complications, significantly impacting an individual’s quality of life.
PAD is a serious condition that increases the risk of cardiovascular events such as heart attack and stroke. Early diagnosis and management are essential to prevent severe complications and improve overall health.
Table of Contents
What is Peripheral Artery Disease (PAD)?
Peripheral Artery Disease is a type of atherosclerosis that affects the peripheral arteries, which carry blood to the arms, legs, and other parts of the body.
The condition often goes undiagnosed because its symptoms can be subtle or attributed to other health issues.
However, if left untreated, PAD can lead to critical limb ischemia (a severe blockage in the arteries of the lower extremities), tissue damage, and even limb amputation.
Symptoms of Peripheral Artery Disease
PAD may be asymptomatic in its early stages, but as the condition progresses, individuals may experience the following symptoms:
- Claudication (Leg Pain): Pain, cramping, or weakness in the legs during physical activity, such as walking or climbing stairs. The pain usually subsides with rest but returns with activity.
- Numbness or Weakness: Reduced blood flow can cause numbness, tingling, or weakness in the affected limbs.
- Coldness in the Lower Extremities: The affected leg or foot may feel colder than the other due to poor circulation.
- Color Changes in the Skin: The skin of the legs or feet may appear pale, bluish, or reddish, indicating inadequate blood flow.
- Sores or Wounds that Don’t Heal: Non-healing wounds or ulcers on the feet or legs can be a sign of advanced PAD.
- Weak or Absent Pulse in the Legs or Feet: A diminished or absent pulse in the peripheral arteries may be detected during a physical exam.
- Hair Loss on the Legs or Feet: Poor circulation can lead to hair loss in the affected areas.
- Erectile Dysfunction: Men with PAD may experience difficulty achieving or maintaining an erection.
Causes of Peripheral Artery Disease
PAD primarily results from atherosclerosis, a condition characterized by the buildup of plaque in the arterial walls. Several factors contribute to the development of PAD:
- Atherosclerosis: It is the most common cause, where fatty deposits accumulate in the arteries, narrowing them and reducing blood flow.
- Smoking: Tobacco use is a significant risk factor for PAD as it damages blood vessels and accelerates atherosclerosis.
- Diabetes: High blood sugar levels can damage blood vessels and increase the risk of PAD.
- High Blood Pressure (Hypertension): Chronic high blood pressure can weaken and damage arterial walls, making them more susceptible to plaque buildup.
- High Cholesterol: Elevated levels of LDL (“bad”) cholesterol contribute to plaque formation in the arteries.
- Obesity: Excess body weight increases the risk of conditions that contribute to PAD, such as diabetes, hypertension, and high cholesterol.
- Sedentary Lifestyle: Lack of physical activity can lead to poor circulation and increase the risk of PAD.
- Age: The risk of PAD increases with age, particularly after 50.
- Family History: A family history of cardiovascular disease or PAD increases the likelihood of developing the condition.
Risk Factors for Peripheral Artery Disease
Certain factors increase the risk of developing PAD:
- Smoking: The leading modifiable risk factor for PAD.
- Diabetes: Diabetics are at a significantly higher risk of developing PAD.
- Hypertension: High blood pressure contributes to arterial damage.
- High Cholesterol: Elevated LDL cholesterol promotes plaque formation.
- Age and Gender: Men over 50 and postmenopausal women are at higher risk.
- Chronic Kidney Disease: Kidney disease is associated with an increased risk of PAD.
Complications of Peripheral Artery Disease
If left untreated, PAD can lead to serious complications, including:
- Critical Limb Ischemia: Severe reduction in blood flow to the limbs, leading to non-healing wounds, tissue damage, and gangrene.
- Heart Attack and Stroke: PAD increases the risk of cardiovascular events.
- Amputation: Severe cases may require limb amputation ( the surgical removal of part of the body, such as an arm, foot, or leg ) due to tissue death.
Diagnosis of Peripheral Artery Disease
Diagnosing PAD involves a combination of medical history, physical examination, and diagnostic tests:
- Ankle-Brachial Index (ABI): A non-invasive test that compares the blood pressure in the ankle to the blood pressure in the arm. A lower ABI indicates reduced blood flow.
- Doppler Ultrasound: Uses sound waves to visualize blood flow and detect blockages in the arteries.
- Angiography: An imaging test that uses contrast dye and X-rays to visualize the arteries and identify blockages.
- Magnetic Resonance Angiography (MRA): A non-invasive imaging test that provides detailed images of the blood vessels.
- Blood Tests: Measures cholesterol levels, blood sugar, and markers of inflammation to assess cardiovascular risk.
Treatment for Peripheral Artery Disease
The treatment of PAD aims to relieve symptoms, improve circulation, and prevent complications. Common treatment approaches include:
Lifestyle Changes:
- Smoking Cessation: Quitting smoking is the most important step to reduce PAD progression.
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins helps manage cholesterol and blood pressure.
- Regular Exercise: Walking and other physical activities improve circulation and reduce symptoms of claudication.
Medications:
- Antiplatelet Drugs (e.g., Aspirin): Prevent blood clots and reduce the risk of heart attack and stroke.
- Cholesterol-Lowering Medications (e.g., Statins): Lower LDL cholesterol and slow plaque buildup.
- Blood Pressure Medications: Control hypertension to reduce arterial damage.
- Medications to Improve Circulation: Drugs like cilostazol can help reduce leg pain and improve walking distance.
Surgical Procedures:
- Angioplasty and Stent Placement: A minimally invasive procedure to open blocked arteries and insert a stent to keep them open.
- Atherectomy: Removes plaque from the artery using a catheter with a rotating blade.
- Bypass Surgery: Creates a new pathway for blood flow around the blocked artery.
Prevention of Peripheral Artery Disease
Preventing PAD involves addressing modifiable risk factors:
- Quit Smoking: Avoid tobacco products to protect arterial health.
- Adopt a Heart-Healthy Diet: Focus on foods that lower cholesterol and blood pressure.
- Exercise Regularly: Engage in moderate physical activity to improve circulation.
- Manage Chronic Conditions: Keep diabetes, hypertension, and cholesterol under control.
- Regular Health Checkups: Monitor cardiovascular health and address risk factors early.
Conclusion
Peripheral Artery Disease is a serious but manageable condition.
Early detection, lifestyle changes, and appropriate medical care can significantly improve symptoms and reduce the risk of complications.
By adopting a heart-healthy lifestyle and managing underlying conditions, individuals with PAD can lead a healthier, more active life.
FAQs on Peripheral Artery Disease
1. What are the 3 signs of peripheral arterial disease?
Three signs of peripheral arterial disease (PAD) include:
- Claudication (Leg Pain): Pain, cramping, or weakness in the legs during physical activity, such as walking or climbing stairs. The pain usually subsides with rest but returns with activity.
- Poor wound healing: Slow healing of sores or ulcers on the legs or feet.
- Weak pulse in the legs or feet: A diminished or absent pulse in the legs or feet.
2. Can PAD be cured?
While there’s no cure for PAD, it’s very manageable. Lifestyle changes like quitting smoking, regular exercise, and a healthy diet can significantly improve symptoms and slow disease progression. In some cases, medications or medical procedures may be necessary to restore blood flow.
3. What is the main cause of peripheral artery disease?
The main cause of peripheral artery disease (PAD) is atherosclerosis, a condition where plaque (a substance made up of fat, cholesterol, and other cellular waste products) builds up in the inner lining of the arteries. This buildup narrows the arteries, reducing blood flow to the limbs.
Other factors that can contribute to the development of PAD include:
- Smoking
- High blood pressure
- High cholesterol
- Diabetes
- Obesity
- Family history of PAD
It’s important to note that while PAD can be a serious condition, it can be managed effectively through lifestyle changes and, in some cases, medical interventions.
4. Can you recover from peripheral artery disease?
Peripheral artery disease (PAD) can be managed, but complete recovery may not always be possible. Treatment focuses on improving symptoms, preventing complications, and halting disease progression. Lifestyle changes like exercise, a healthy diet, quitting smoking, and medications are vital. In some cases, procedures like angioplasty or surgery may be required to restore blood flow.
5. What is the final stage of PAD?
The final stage of peripheral artery disease (PAD) is called critical limb ischemia (CLI). It occurs when blood flow to the limbs is severely reduced, causing intense pain, ulcers, sores, or gangrene. At this stage, there is a high risk of infection, tissue death, and possibly limb amputation if not treated promptly and effectively.
6. How to test for PAD at home?
To test for peripheral artery disease (PAD) at home, check for signs like leg pain while walking, numbness, or cold feet. You can also perform the “ankle-brachial index” test using a blood pressure cuff and a home Doppler device to compare the blood pressure in your ankle and arm. Consult a doctor for accurate diagnosis and treatment.
7. What exercise is good for peripheral artery disease?
For peripheral artery disease (PAD), walking is one of the best exercises. It helps improve circulation and strengthen the muscles without straining the heart. Start with short, gradual walks, increasing the duration as tolerated. Other beneficial exercises include cycling and supervised strength training. Always consult a doctor before starting an exercise routine.
8. What is the best position to sleep in with peripheral artery disease?
For individuals with peripheral artery disease (PAD), sleeping with the legs elevated can help improve blood flow. Lying on your back with your legs elevated slightly above heart level, using pillows, can reduce swelling and promote circulation. Avoid sleeping with legs dangling off the bed, as it may worsen circulation issues. Always consult a healthcare provider for personalized recommendations.
9. What organs are affected by peripheral artery disease?
Peripheral artery disease (PAD) primarily affects the legs and feet, leading to reduced blood flow and oxygen supply. However, it can also have an impact on other organs due to its connection to atherosclerosis. PAD increases the risk of heart disease, stroke, and kidney problems, as it can affect blood vessels throughout the body, including those supplying the heart, brain, and kidneys.
10. What foods should you avoid when you have PAD?
When managing peripheral artery disease (PAD), it’s important to avoid foods that can worsen blood flow and increase cholesterol. These include:
- Trans fats (found in fried and processed foods)
- Saturated fats (like red meat, butter, and full-fat dairy)
- Refined sugars (sugary snacks and drinks)
- High-sodium foods (processed foods, canned soups)
Instead, focus on a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins.